Feature
PEPFAR’s new goal: Ending HIV by 2030
John Robert Engole is not a household name, but the world should celebrate his 54th birthday later this year. His being alive and healthy is testament to an astonishingly effective global health effort. Reaching middle age appeared unlikely for him in 2004, when he arrived at a clinic run by Reach Out Mbuya, a faith-based NGO, in the suburbs of Kampala, Uganda’s capital. Engole was very weak and had the severe tuberculosis common for HIV/AIDS patients, recalls Margrethe Juncker, a doctor and co-founder of Reach Out. A test showed Engole’s CD4 level was at 1, meaning his immune system could not defend him against infections and harmful invaders. He also had an itching rash, a visible sign of late-stage HIV in a city where so many died from the virus that coffins were sold on street corners.
But Engole came to the clinic on the first day of a new U.S. government program to fight HIV, the President’s Emergency Plan for AIDS Relief, or PEPFAR. His timing, plus the severity of his illness, resulted in his becoming the first person treated under PEPFAR, which made antiretroviral therapies available in places that previously had little to no access. The drugs “created a Lazarus effect,” says Juncker. “We were seeing patients dying at the clinic and there was nothing we could do. The dying stopped after PEPFAR provided [antiretrovirals].” Juncker calls the program a “miracle” that changed the future for many Ugandans.
Today, Engole’s viral load is suppressed, meaning HIV is not detectable in his system. “I am healthy, married, and upgrading my education,” he says. He teaches secondary school in Amuria district, northeast of Kampala, and pastors a Pentecostal Assemblies of the World Church congregation in his village. He has six children, the oldest one attending a university, and is himself pursuing a master’s degree in theology with the hope of getting a PhD. “My dream is to become a university professor,” he says.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
That dream would have been impossible before President George W. Bush announced PEPFAR in 2003. HIV was devastating families, communities, and economies worldwide—particularly in sub-Saharan African countries, where fewer than 50,000 people had access to antiretroviral therapy. Today, PEPFAR has saved over 25 million lives across more than 55 countries on four continents. In Uganda, one of its most successful initiatives, PEPFAR is estimated to have prevented nearly 600,000 HIV-related deaths and 500,000 infections, 230,000 of them among HIV-exposed infants. In its first year, 2004, 66,500 people with HIV worldwide received treatment thanks to PEPFAR. Last year, that number was 20 million—1.3 million in Uganda.
John Nkengasong, U.S. Global AIDS Coordinator and the head of PEPFAR, which is part of the U.S. Department of State, says PEPFAR’s goal is to end the HIV/AIDS pandemic by 2030. “My expectation is our partner governments will lead the response, keeping communities at the center,” he says.

Protesters in Entebbe, Uganda challenged President Bush on his arrival to tout PEPFAR in July 2003. The program would help to lower treatment costs.
J. Scott Applewhite / AP Photo

John Robert Engole, right, the first person treated under the PEPFAR program, at the Reach Out Community Health Initiative in suburban Kampala in 2012.
Rodney Muhumuza / AP Photo
PEPFAR, at $110 billion and counting since its inception, is the largest financial commitment by any nation to address a single disease. It has also helped the countries it works with become less dependent on aid, and to build up their health care sectors for better care. To that end, it will invest $1.1 billion to train 325,000 health workers across Africa, and has pledged to buy 15 million African-made HIV tests in 2025.
The program has transformed public health in many countries, says Phyllis Kanki, who created and directed the AIDS Prevention Initiative in Nigeria and is now a professor of health sciences at the Harvard T.H. Chan School of Public Health. She says it has expanded treatment capacity and bolstered local scientists, who have done work that has improved health care for HIV and other diseases. And, “the speed at which PEPFAR made a difference is probably not something that people think about,” Kanki adds, but it was “a game changer.”
PEPFAR grew out of scientists trying to stop a scourge. Some of the most important work came from a collaboration between Botswana—among the countries most afflicted by AIDS—and Harvard. The Botswana-Harvard AIDS Institute Partnership was established in 1996, and it was here that Myron “Max” Essex, a virologist at the Harvard Chan School, was among the first to suggest a retrovirus caused AIDS. Researchers also studied how to prevent mothers from transmitting HIV to their babies and ran one of the largest trials examining how treatment regimens affected outcomes. The Institute’s work created Botswana’s template for bringing antiretroviral treatments to its citizens, says Tendani Gaolathe, a physician and project director at the Institute.
Other scientists were asking questions about who was suffering from HIV and why. Laura Guay, a research professor at George Washington University and vice president of research at the Elizabeth Glaser Pediatric AIDS Foundation, went to Uganda for the first time in 1988, with a host of questions. “They were seeing a lot of women and children with HIV, but we didn’t understand very much about it,” Guay says, including its epidemiology, the prevalence in different populations, and transmission rates in Uganda compared to the U.S.
Guay, a pediatric infectious disease physician, started out by developing studies testing pregnant women in prenatal clinics for HIV, which previously had not occurred. She wanted to understand how often they transmitted the disease to their fetuses. Working at Kampala’s Mulago National Referral Hospital, the largest public hospital in Uganda, she found about a third of pregnant women were infected with HIV. “We were seeing a lot of maternal deaths, infant deaths,” Guay says, “and it was clear that we had to do something to prevent mother-to-child transmission.”
Meanwhile, wealthy countries were rapidly implementing the antiretroviral AZT (azidothymidine), after studies showed it yielded a 75 percent decrease in mother-to-child-transmission. But with a price of $1,000 and a regimen of five doses a day starting in the second trimester, AZT was not feasible in Uganda, where expectant mothers often did not have their first prenatal visit until well into the second trimester.
Such stark discrepancies spurred work to find more effective ways to treat mothers in places with limited medical infrastructure. That led to HIVNET 012, a seminal trial of two short-course antiretroviral drugs that started in late 1997 in Uganda. One drug, nevirapine, cut mother-to-child transmissions almost in half with one dose. It could be used to treat babies born with HIV. It was affordable and could be administered in places with limited resources.
After the study was published in 1999, it galvanized the creation of programs to prevent HIV transmission from mothers to their babies. “That study was the first time we learned that you could use antiretroviral drugs to prevent infection and transmission, not just treat it,” Guay says. “It really changed the conversation” about HIV testing, which became routine for pregnant women in Uganda.
It also prompted the U.S. government to commit about $100 million to preventing mother-to-child transmission. This was the first step toward the creation of PEPFAR.
It would be a lifesaver for Jane Nalwadda, another patient at the Reach Out clinic on the first day treatments started in 2004. She’d discovered she had HIV in 1992, when she gave birth to a son who was HIV positive. By 2004, she was very ill—“I was hopeless,” Nalwadda says. “The treatment helped me and my son stay alive.” Today, she is 56 and her son is healthy. Without PEPFAR they would probably both be dead.

Laura Guay, pediatrician and HIV researcher (standing), researching how the disease was transmitted from pregnant women to their babies in 1990 in Kampala, Uganda.
Courtesy of Laura Guay

A patient at Reach Out Mbuya Community Health Initiative receives care from Precious Aine, one of the clinic’s community and antiretroviral therapy/TB support staff.
Annet Nakibuuka / Reach Out Mbuya
For all the lives saved, PEPFAR may be even more important for the work it has sparked to strengthen health systems around the globe. Laboratories have been built, health care workers trained and supported, and disease-monitoring systems bolstered. These efforts have been used to fight other health crises, including COVID-19. The South African laboratories that identified new COVID variants were built as part of the PEPFAR-backed effort to fight HIV. Testing and community outreach programs used to fight COVID in many countries were initially part of the fight against AIDS.
The regular, consistent data reporting PEPFAR mandated also had broad ripple effects. In countries such as Botswana, Nigeria, and Tanzania, this reporting structure spurred broader use of electronic medical records.
Botswana may be the prime example of a country that has built a stronger, self-sustaining public health system because of its work with PEPFAR. “Botswana invested its own resources and tried to build this up using primary health care systems,” says Matshidiso Moeti, World Health Organization regional director for Africa. By dedicating its own funding—the government puts up about 80 percent of total HIV spending in the country—it improves the likely sustainability of its fight against AIDS.
PEPFAR’s investments in the Botswana Harvard AIDS Institute, with concurrent investments by the Botswana Ministry of Health & Wellbeing, funded training and capacity building for prescribing and administering antiretroviral therapies. The Institute’s Gaolathe says this close involvement has meant a continual refining of where to put resources—for instance, shifting from training nurses and lab technicians to developing a pharmacy training program. The ultimate result: In 2022 Botswana reached the 95-95-95 target, where 95 percent of people with HIV know they have it, receive antiretrovirals, and have achieved viral suppression.

Sarah Nassolo (center) and her family meet with U.S. Secretary of State Hillary Rodham Clinton at Reach Out Mbuya, a health clinic that does HIV/AIDS community outreach.
Jacquelyn Martin / AP Photo

Jakaya Kikwete (left), former president of Tanzania, listens to former President George W. Bush at a PEPFAR anniversary event in February 2023.
J. Scott Applewhite / AP Photo
The key to PEPFAR’s success has beenits longevity and consistency— “It isn’t a pro-gram that operated for five years and then went away,” says Kanki. The U.S. has said, however, it would like to reduce its spending on PEPFAR. And the program’s goal is to put itself out of business by eliminating HIV as a global public health threat by 2030. This outcome is ambitious but not impossible. Between 2015 and 2022, the percentage of people receiving HIV treatment through PEPFAR who have the virus under control rose from 80 percent to 95 percent.
Still, sustainability remains a significant hurdle for individual countries. Uganda is considered a success story, but its outcomes might be different without PEPFAR’s aid. Last year, Uganda’s government spent 300 billion Ugandan shillings ($80 million U.S.) on HIV treatment, far less than the 2 trillion Ugandan shillings ($534 million U.S.) needed. “We still need partners until our economy is strong enough to support such an investment,” says Vincent Bagambe, director of planning and strategic information at the Uganda AIDS Commission. Bagambe notes the government’s entire budget in 2021 was about $4 billion U.S., and HIV is not the only disease it needs to fight.
Cultural factors also can affect treatment. Uganda may pass a law that imposes severe penalties against homosexuality, including any form of support for LGBTQ+ people. As of press time, Ugandan President Yoweri Museveni had sent the bill back to parliament for what he termed “improvements.” In response, PEPFAR delayed a planning meeting for its Uganda efforts, issuing a statement that it needed to assess the impact of “the evolving legislation and broader environment” in Uganda.
In addition, there remain gaps in HIV prevention. Bagambe says in Uganda about 5,000 children a year are still born with HIV. For more than half of them, their mothers contracted the virus after they became pregnant, or even while breastfeeding.
Meanwhile, large numbers of people with suppressed HIV are now in their 40s and 50s and starting to suffer chronic health issues, such as diabetes and hypertension. PEPFAR needs to pivot, says the WHO’s Moeti. “If I am PEPFAR and I kept you alive for 20 years, I don’t want you to die now of diabetes because I can’t expand a bit to include you in what I am doing,” she says.
Such a shift would be a natural step, says Guay, given PEPFAR’s effectiveness in building out HIV services. It could extend these services and integrate them to fight a variety of illnesses. HIV will remain its focus for now, Nkengasong says. “We have to accelerate our efforts to end the HIV/AIDS pandemic to sustain the gains we’ve achieved to date,” he says. “We don’t know what the next emerging disease threat will be, but the best way to prepare for the unknowns is to address the knowns. HIV/AIDS is a ‘known.’”
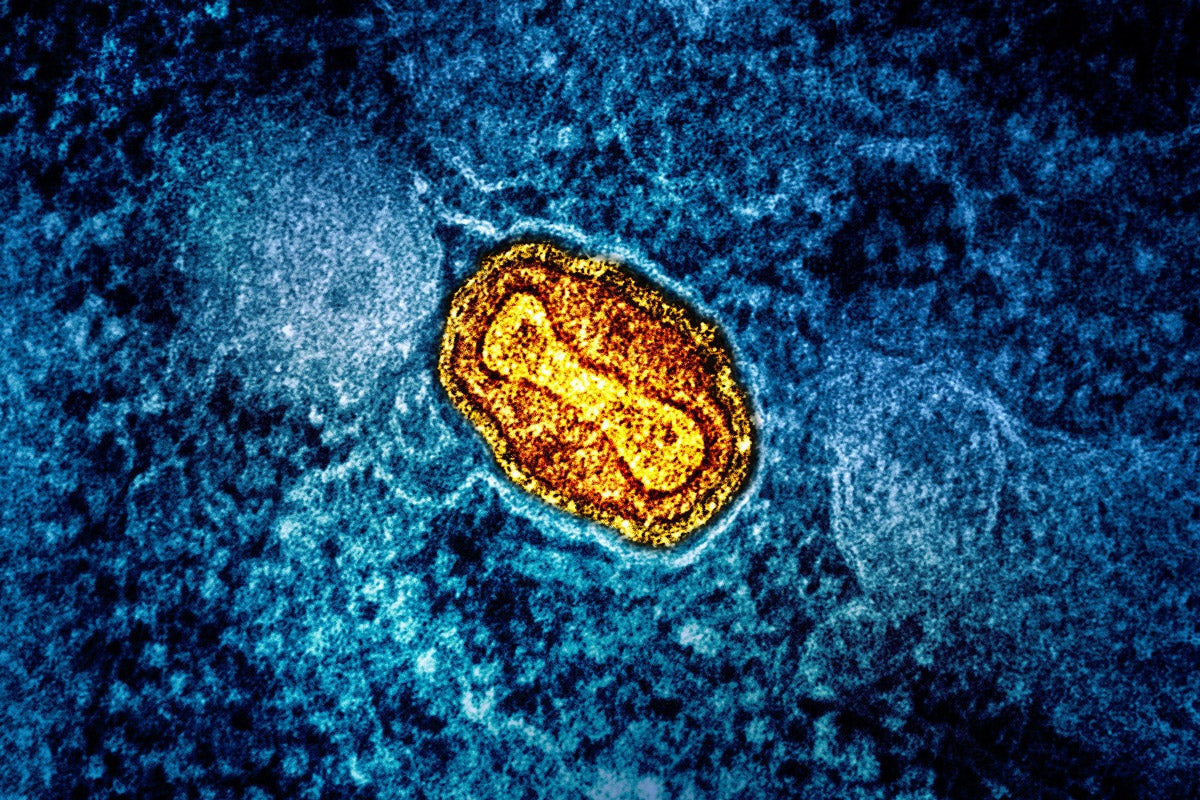
Top image: A President’s Emergency Plan for AIDS Relief (PEPFAR) banner at a World AIDS Day event in December 2022. Photo: Jonathan Ernst/Pool Photo via AP Photos