Feature
Precision health’s tantalizing promise for changing outcomes
Public health runs on data. One early effort was London’s Bills of Mortality, which in 1592 began a weekly report of data on causes of death for everyone in the city. The data was woefully incomplete by modern standards—causes of death included everything from plague to “Kingsevill”—but the concept was sound. Three centuries later, the critical importance of data in public health was solidified when proto-epidemiologist John Snow went door-to-door during one of the city’s many cholera outbreaks to collect data about the role of contaminated water in disease transmission.
Over time, public health data has grown more sophisticated. Death certificates can’t just read “toothache,” and detailed GIS mapping has replaced Snow’s shoe-leather epidemiology. That’s just the start: Thanks to the ever-decreasing costs of DNA sequencing, even genetic information has moved into the public health domain.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
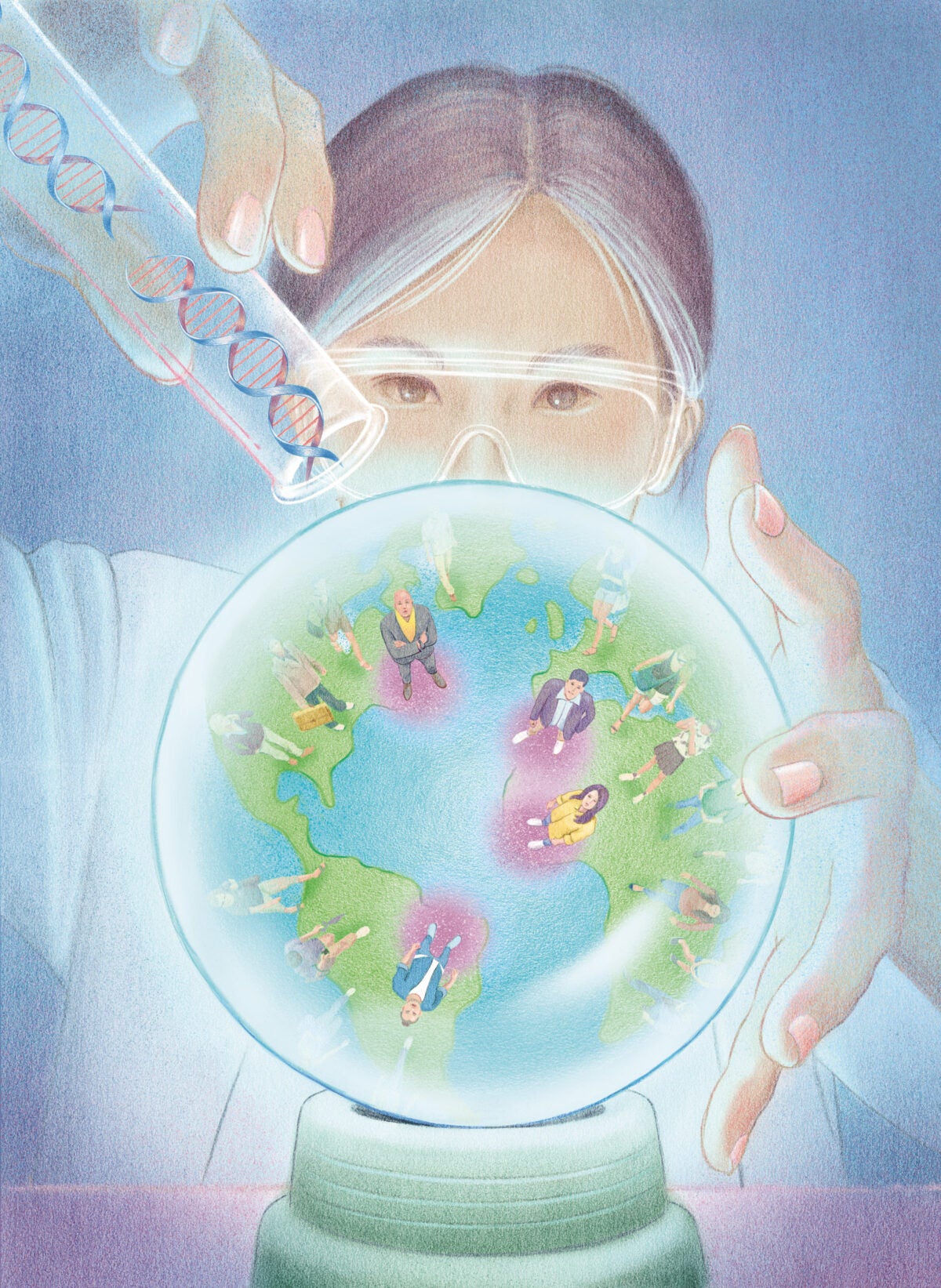
This data deluge has brought new opportunities for public health—including an unprecedented ability to identify needs at a hyper-local level and tailor interventions accordingly. That’s a significant mind-shift for public health leaders who are accustomed to thinking on a population scale. Indeed, part of the field’s attractiveness has always been its near-universality. Safe drinking water benefits everyone. So do clean air, vaccines, and smoking cessation. But it’s become increasingly clear that not everyone benefits equally from the same intervention. Someone at increased genetic risk for breast cancer, for instance, might benefit far more from regular mammograms than a neighbor at low risk. And that realization is fueling the burgeoning field of precision public health.
In precision medicine, “we fingerprint what’s going on in the body, all the way from molecules to full-blown disease,” says Maureen Lichtveld, dean of the School of Public Health at the University of Pittsburgh. “The only way to get to sustained health is by doing the same kind of fingerprinting at the community level.”
The idea of personalized medicine grew out of the effort to sequence the human genome. By the time it was first published in 2003, drug developers had spent years exploring how to tailor medicines to an individual’s unique genetic sequence. This n-of-one approach was, in many ways, the polar opposite of universal public health interventions. But as precision medicine inched its way into primary care, some public health scientists, including Muin Khoury, a genomic epidemiologist at the Centers for Disease Control and Prevention, began to wonder whether they could adopt the tools used in precision medicine. Inspired by the strategy and ethos of precision medicine—the right treatment to the right patient at the right time—Khoury wrote a CDC blog post in March 2015 that the new field “goes beyond individualized treatment of sick individuals. The word ‘precision’ in the context of public health can be simply described as improving the ability to prevent disease, promote health and reduce health disparities in populations.”
In some sense, precision public health is merely an updated version of the field’s familiar strategy of using data to guide interventions to improve well-being. But the massive quantities of data that scientists now have at their fingertips have opened new possibilities—once they can learn how to harness the windfall. The skills needed to parse genomic data “are the same skills we need to integrate transportation data and air pollution data,” says Lichtveld, who is working to boost Pitt’s School of Public Health data science portfolio in anticipation of students needing to support precision public health.

Hundreds of healthy-seeming newborns have had their genomes sequenced as part of BabySeq. More than one in 10 were found to have unexpected disease risks.
Many precision public health projects have been enabled by the plummeting price of genetic testing. Caitlin Allen, a social and behavioral scientist at the Medical University of South Carolina, has helped to launch a project called In Our DNA SC, which is recruiting 100,000 people in South Carolina to provide genomic screening for hereditary breast and ovarian cancer syndrome, Lynch syndrome (the most common hereditary colon cancer), and familial hypercholesterolemia (genes that affect the body’s ability to prevent cholesterol build-up). Only a small proportion of individuals at high genetic risk for these conditions know their status, which means they are missing out on recommended screenings. The project’s goal is to identify people at high-risk for these cancers that are missed by traditional screening methods, so they can be connected to preventive services. Allen’s team also intends to develop targeted messaging to individuals at high genetic risk and work with primary care providers across South Carolina to include genomic testing in basic patient care.
Other research projects cast an even wider net. Robert Green, a medical geneticist and director of Genomes2People, says “We’re overdue for a population-based approach to genomic medicine.” He directs a program called BabySeq that aims to measure the risks and benefits—both social and medical—of sequencing the genomes of newborns who seem healthy. Hundreds of infants have had their genomes sequenced as part of BabySeq, and more than one in 10 had unexpected disease risks. That information resulted in some of their relatives getting tested, too.
Green also leads the Precision Population Health initiative at Ariadne Labs, a joint initiative of Harvard T.H. Chan School of Public Health and Brigham and Women’s Hospital. The Initiative partnered with Beaumont Hospital System in Michigan (since merged to form Corewell, the largest system in the state), which wants to give its racially and financially diverse population of primary care patients the option to have their genome sequenced. The goal: Transform genomic sequencing from a diagnostic tool for patients who already have an illness to one that can find known, treatable diseases that have not produced symptoms yet. “It’s possible to screen not just for one disease at a time, but to screen for dozens, hundreds, or even thousands. That, to me, feels like a public health approach,” Green says.
One potential hurdle: Information in databases that inform genomic risk is disproportionately from individuals with European ancestry. The National Institutes of Health aims to address that concern with its All of Us program, which seeks to create one of the most diverse databases in history by collecting genomic and health data on one million people across the U.S. Other countries are also trying to lessen these disparities.
In Argentina, anthropologist Rolando González-José is coordinating PoblAr, an effort by the Ministry of Science, Technology and Innovation to capture genetic, social, and biomedical information from thousands of volunteers across the country. The goal is to create a genetics reference tool that contains the width and breadth of the country’s diversity, and pair it with epidemiological and phenotypic data to aid in the development of public policies and disease interventions. Gathering data about lifestyles, access to health systems and education, and other practices means “this is about precision health,” González-José says.
Despite these efforts, some critics of precision public health worry that these pricey, tech-heavy programs will further widen the gap between the haves and have-nots. Ina world where people lack access to safe drinking water and essential medications, DNA sequencing for all can seem like a misplaced priority. But a growing number of initiatives are showing that precision public health can be effective, even in resource-limited settings.
Having enough to eat is one of the most basic human needs. Yet around the world, one in three children under five experiences severe malnutrition. In India, more than one-third of children under five show at least one sign of chronic undernutrition—wasting (low weight-for-height), stunting (low height-for-age) and underweight (low weight-for-age). Given India’s size—1.27 million square miles—and population of 1.4 billion, however, these measures vary widely.
S.V. Subramanian, professor of population health and geography at the Harvard Chan School, wanted to know how much childhood undernutrition varied within India, which has hundreds of districts, averaging 1.3 million people each. This wasn’t just idle curiosity: He had noticed that, although childhood malnutrition existed throughout the country, not every location was affected equally. More data, he realized, might help leaders funnel efforts into the most impacted villages.
So, with an international team of scientists, Subramanian set out to map undernutrition for each of India’s nearly 600,000 villages. Using data from a range of sources, Subramanian and colleagues built a machine learning model to estimate the prevalence of stunting, underweight, and wasting in each village. What resulted was an April 2021 PNAS paper that showed prevalence of growth stunting ranged from under 5 percent in some villages to more than 70 percent in others, averaging out at 37.9 percent. It was the first such detailed calculation of this data across India—and it made an incontrovertible case that interventions ought to be targeted to certain regions, and with a high degree of urgency. “This is not the estimate of undernutrition, this is an estimate of undernutrition,” Subramanian cautions. “You need a fair degree of precision to reach the right person, the neediest person, the neediest family, the neediest village,” and the data quality needs to improve to get that granular. But for now, “we can at least get a broad sense of what might be happening at the granular level.”
Using data to assess need and target interventions also proved critical during the COVID pandemic, especially since decades of funding cuts across U.S. public health departments left them without resources to deploy contact tracing and rapid testing. In Davis, California, a city just west of Sacramento, the community wanted a targeted approach for under-resourced areas and those with high transmission. It happened that the data-driven approach the University of California, Davis, devised to get students safely back on campus was something the city could adapt.
Brad Pollock, a professor of epidemiology at the University of California, Davis, was involved in organizing an initiative called Healthy Davis Together to apply a precision targeting approach to their public health interventions. The program data documents clear successes: Over 16 months, the targeted interventions prevented over 4,000 cases of disease, reducing case counts by 60 percent.
The effort was cost-effective, too. Healthy Davis Together spent $34.1 million but estimated that its work cut expenditures in lost wages, hospital care, and averted deaths and disabilities related to COVID, with total savings amounting to $112.7 million.
But Pollock also says response efforts were hamstrung by data bottlenecks along the way. He needed a firehose of information but got a mere trickle, in part thanks to California’s incomplete geographic information on Davis residents with positive test results. Data, he says, “should be used for everything we do. So why don’t we? It’s not because we don’t want to. It’s because we don’t have the data.”
To give more countries and institutions access to precision analyses, the Rockefeller Foundation has partnered with the World Bank, Gavi, the World Health Organization, and UNICEF to develop precision public health tools for some of the world’s most underserved populations. The $100 million project, which was launched in late 2019, is also designed to develop best practices for building and implementing digital public health infrastructure.
“You can put as many tools out there as you want. You can support all the analytics that you want, but if you don’t have a functioning health system, it’s difficult for the health system to utilize those data analytics to affect change,” says Greg Kuzmak, director of digital health at the Rockefeller Foundation.
“Even for applications in genomics and public health that can save lives today, implementation is not happening fast enough,” agrees Khoury.
Yet technology alone isn’t an all-powerful solution. Big Data might be able to identify where community health workers are most needed, but it can’t replace the workers themselves—or eliminate the need for trusted communication from respected local officials. In other words, the precision public health revolution will still need plenty of foot soldiers.
“Technology is an enabler,” says Manisha Bhinge, managing director of global networks and partnerships with the Pandemic Prevention Initiative at Rockefeller. “We still need an analog system. There’s a behavioral component that is agnostic of technology, and it’s a human factor.”