From the editor
Our top stories of 2023
Tens of thousands of you have visited Harvard Public Health this year to read our original reporting, opinion essays, book reviews, interviews, and more. Here’s a selection of your favorites—and ours.
As climate change erodes land and health, one tribe fights back

Photo: Edmund D. Fountain
In the Louisiana bayou, Native American tribes are living in what journalist Barry Yeoman calls “a feedback loop of destruction.” Between decades of shipping-friendly policies that have weakened watersheds and the more recent extremes from climate change, farming is often futile, flooding is common, and the future for one local Native American tribe feels bleak.
But the young chief of the Grand Caillou/Dulac Band of the Biloxi-Chitimacha-Choctaw hopes that, together with leaders from other area tribes, he can start to turn things around.
We can’t stop at water—it’s time to kick PFAS out of our makeup

Source image: Amy Shamblen / UnSplash
“Tens of millions of consumers unknowingly rub products containing these hazardous chemicals into their skin and hair every day,” writes Shruthi Mahalingaiah. A physician and professor, Mahalingaiah uncovered traces of more than 1,700 environmental chemicals in the menstrual blood samples her lab studied. The toxic chemicals known as PFAS can cause cancer, obesity, decreased fertility, and a weakened immune system—and show up in makeup and period products.
Author Clancy Martin on surviving suicide attempts

Book cover: Courtesy of Pantheon Books
Acclaimed novelist Clancy Martin wrote How Not to Kill Yourself because it was the book he most needed. “All the memoirs about suicide that I read didn’t tend to offer practical advice on how to help people suffering from suicidal ideation,” he told HPH in an interview. A blend of memoir and philosophy, his book aims to share some advice from his readings of philosophy, the letters he’s exchanged with others over the years, and from his own life.
Paid family leave needs to expand its definition of “family”

Illustration: Nicole Xu
Not many states offer paid family leave to people caring for aging relatives—and most of them limit eligibility to immediate family members.
But Black women “are more likely to age without living family members than White women and men,” writes reporter Constance Sommers. They’re also more likely to rely on friends or distant relatives.
“We need to expand the definition of ‘family’ if you want to be equitable for the Black community,” Carlene Davis, who runs a nonprofit that serves aging people in Los Angeles, told Sommers. “The Black community needs to define who family is for them. For us, family is whomever I trust, who says they’re going to take care of me.”
Processed foods are making us sick. It’s time for the FDA and USDA to step in.

Photo illustration: Mary Delaware / Harvard Public Health
Jerold Mande, an adjunct professor of nutrition at the Harvard T.H. Chan School of Public Health, points a finger at processed foods for the enormous number of U.S. deaths from chronic diseases like obesity, diabetes, heart disease, and cancer. He also calls for a “paradigm shift” at the Food and Drug Administration and the U.S. Department of Agriculture, saying they “must work together to design a 21st century food safety system to protect us not just from acute cases of food poisoning but also from the deadly toll of chronic exposure to ultra-processed food.”
Can Medicaid solve the “Minnesota Paradox?”

Illustration: Noah Lawrence-Holder
“Minnesota often tops lists of places with great health and educational attainment, but my review of more than a decade of data showed that within Medicaid, there are huge disparities in access and outcomes between White community members and our community members of color, particularly Black and American Indian,” writes Nathan Chomilo, a pediatrician and the medical director of Minnesota Medicaid.
His team set out to fix that. Their most important tool? Dialogue.
Tuberculosis, not COVID-19, is the plague of the century

Photo illustration: Mary Delaware / Harvard Public Health
“For people who don’t live in rich nations with ample access to vaccines and effective treatments, the flaws in the global health system’s pandemic response existed long before SARS-CoV-2 made landfall,” writes Vidya Krishnan, author of The Phantom Plague.
One critical flaw is the neglected funding for the prevention and treatment of tuberculosis—even though roughly two billion people are living with latent TB infections. Krishnan argues that improving diagnostics and phasing out old medicines are crucial next steps.
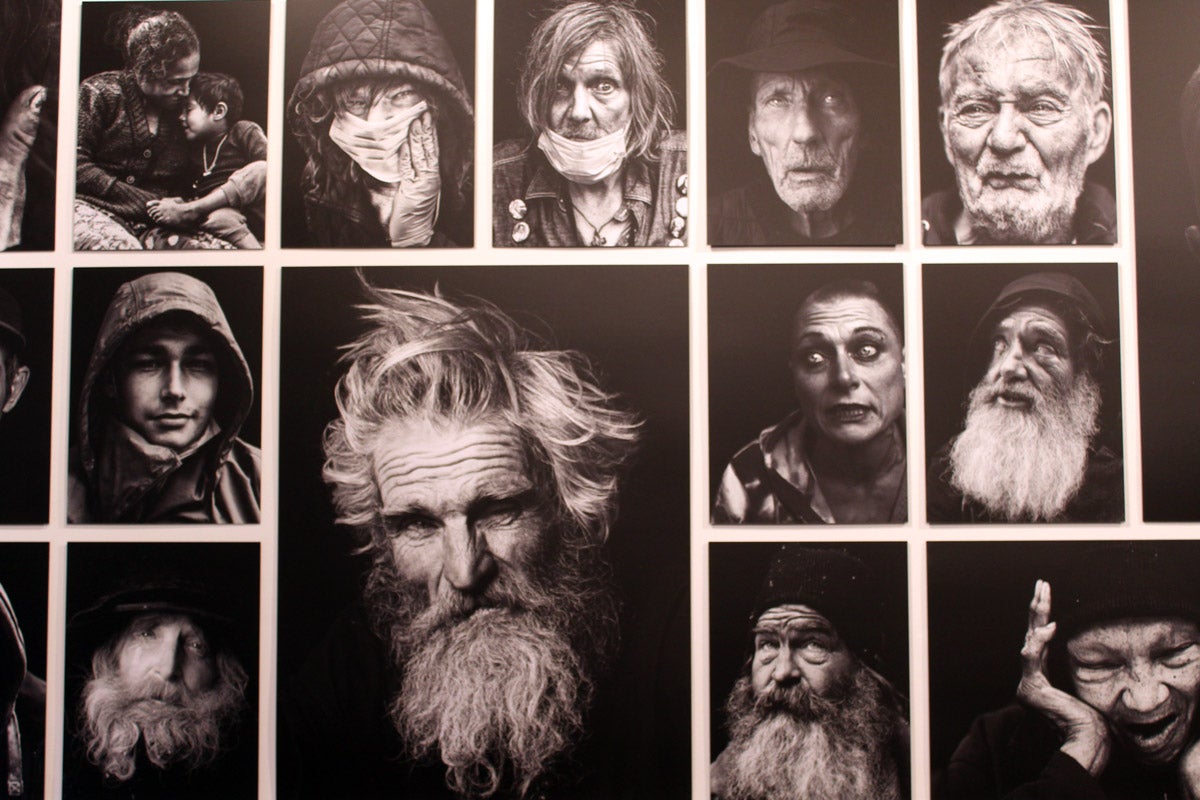
The fall of global health’s benevolent dictatorships
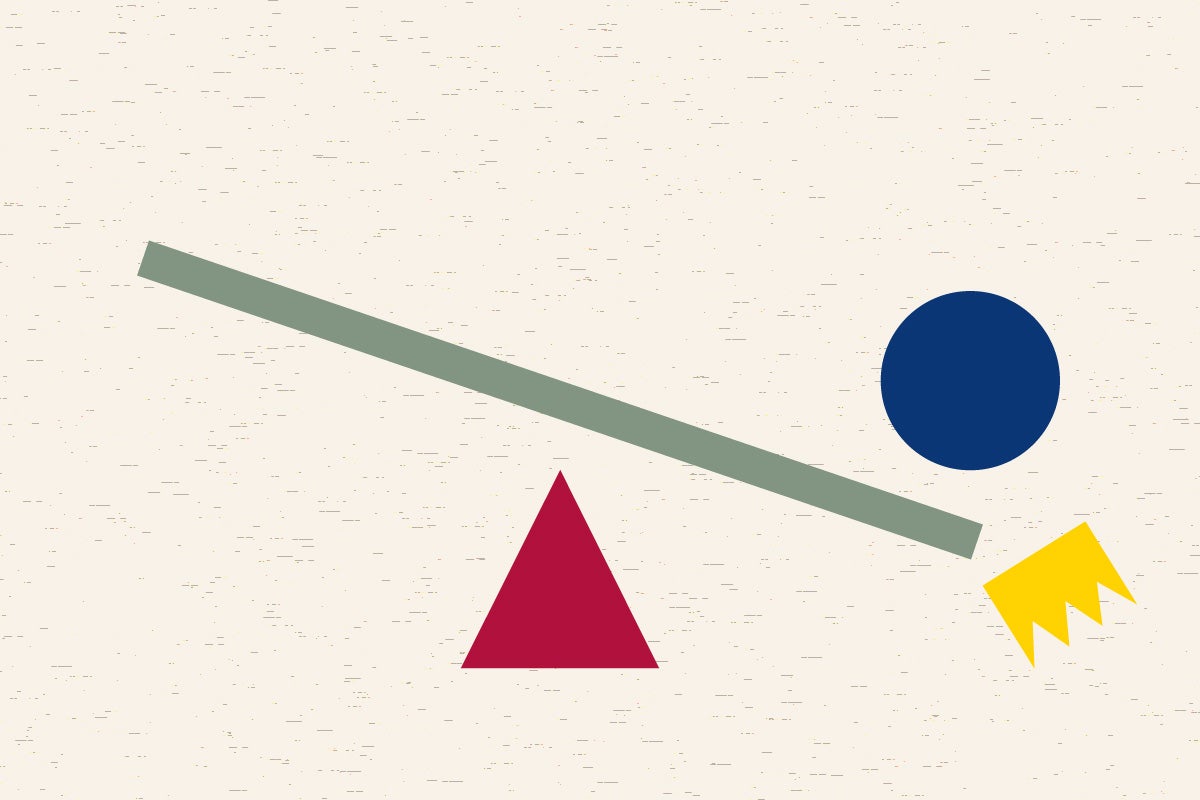
Illustration: Mary Delaware
It’s no secret that global health initiatives often failed to get vaccines and other COVID-related supplies to people around the world in a timely fashion. “Those failures accelerated an ongoing rethink by NGOs on how to more effectively distribute aid and resources,” writes Nigerian science journalist Paul Adepoju. He pinpoints a new era in global health efforts: Collaboration and partnerships are putting funding more directly in the hands of local partners. The shift upends decades of practice, and it’s far from easy—but in Ukraine, India, and parts of Africa, systemic change is already taking off.
The path to universal health care access in South Africa

Source image: filo / iStock
“South Africa is mired in a deeply inequitable two-tiered system,” writes global health reporter Andrew Greene. “An underregulated private sector serves a minority of the country but employs nearly 80 percent of its doctors and specialists. The rest of South Africa—roughly 50 million people—relies on an overstretched, understaffed public system.”
Now, the government is trying to change that. South Africa’s legislature is laying the legal infrastructure for a universal health system. Critics say it’s unclear how the government will foot the mammoth bill, but supporters say capturing profits from the private sector and reinvesting them in public health will go a long way toward the country’s post-apartheid constitutional guarantee of health care for all.
I was alone and sick of it. Technology to the rescue?

Photo: Kent Dayton
In one pre-pandemic study, 60 percent of Americans reported feeling unattached to others—in other words, lonely. Some people are using robo-companions and technology assistants to ease those feelings.
Maura Kelly, who counts herself among the lonely, gets the appeal. “[L]oneliness is excruciating. I am younger than the nursing home set, and skeptical a robot could substitute for human companionship. But trying one would surely be less painful than most of the Hinge dates I’ve been on lately. Why not?”
(It didn’t work out quite as planned.)
North Carolina’s radical Medicaid reinvention

Photo: Andrea Bruce
Eighty percent of what affects our health happens outside of a medical setting. Medicaid is taking notice: Increasingly, states are using Medicaid funding to address the social determinants of health, like housing and poverty. In North Carolina, the $650 million Health Opportunities Pilot supports qualified Medicaid recipients with home renovations, transit passes, auto repairs, and fresh food deliveries.
Dawn Verret, who was hospitalized for malnutrition, neuropathy, and pneumonia after losing her job at the start of the pandemic, said the home renovations Medicaid covered were life-changing. “You have no idea what being able to take a shower every day does to your self-esteem,” she told reporter Melba Newsome. “I really believe that I’m gonna be able to take care of myself and get stronger because I feel like I’m my best self.”