People
“The Forgotten Girls” of the American Ozarks
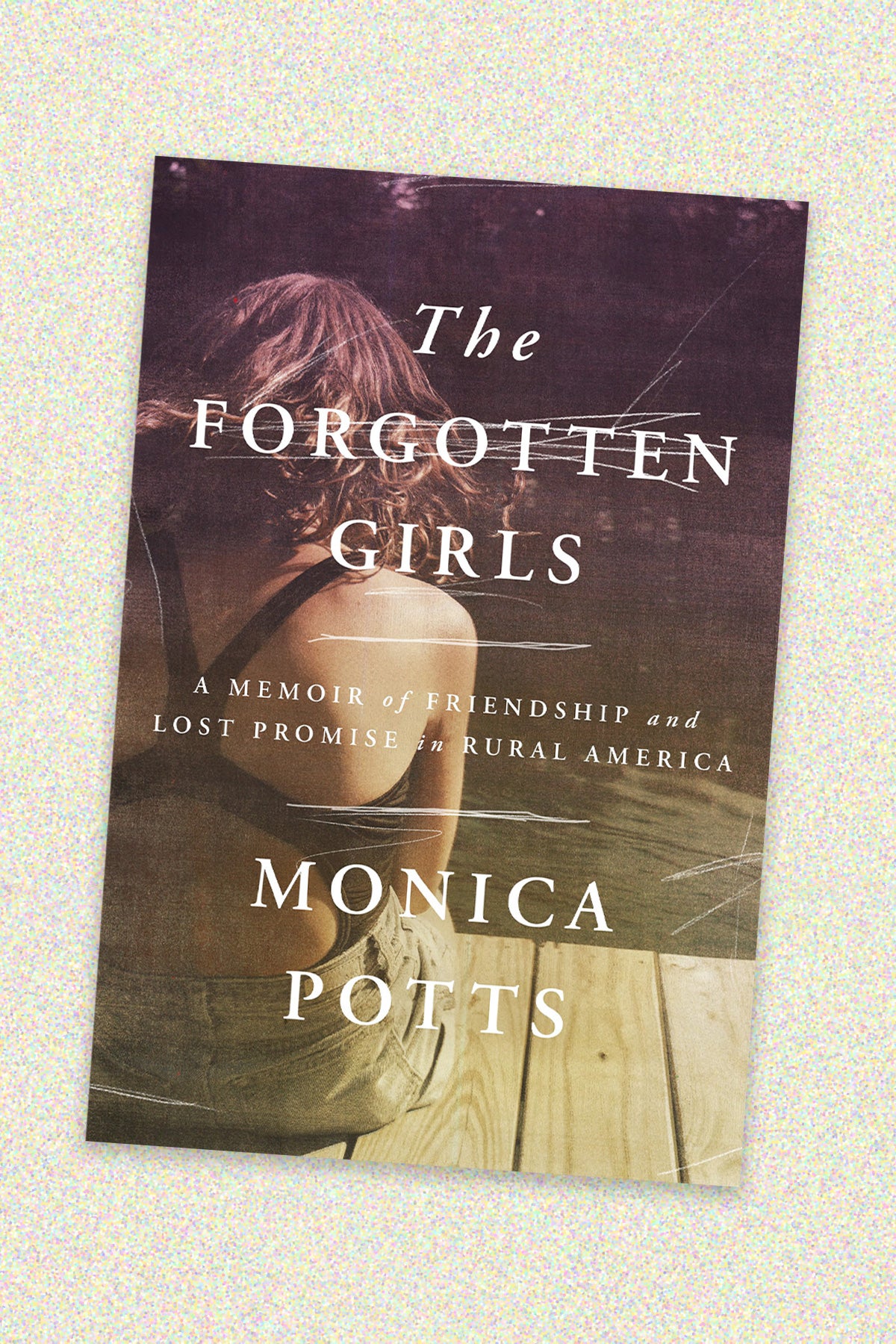
Poor Americans are dying up to 20 years younger than their wealthier counterparts—the biggest gap in 40 years. For Monica Potts, a senior politics reporter at FiveThirtyEight and author of The Forgotten Girls, a book about dying young in rural Arkansas, those are more than just statistics.
Potts knows the people behind the numbers, especially the women. Though she carved out a career for herself in the upper ranks of the journalism world, she grew up working class in the foothills of the Arkansas Ozarks, where the median household income was $40,000 and life expectancy is 74 years. To better understand why her childhood friends seemed fated to die young, she returned home to write about the people she’s known all her life.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
The resulting memoir is a story of contrasts. Potts tells her own story alongside that of her childhood best friend, Darci—who struggles with a substance use disorder and homelessness. In following Darci’s story, Potts considers how abuse and neglect go unacknowledged and untreated, and how generational trauma, teen pregnancies, and vaccine hesitancy add up to a deepening health crisis in rural America. The interview was edited for length and clarity.
Kelly: Why did you write this book?
Potts: We think we’ve achieved so much advancement in gender equality in America, and we have, but there is still a lot of resistance to all kinds of equality, including gender. I wanted to shed light on that. But also, my friend Darci wanted to help people who found themselves facing challenges similar to the ones that she’s faced.
Kelly: How has the overturning of Roe made things worse for women’s health in rural America?
Potts: Arkansas and nearby states like Mississippi and Louisiana have the highest rates of teen pregnancies in America. [According to the latest CDC data, Arkansas had the highest teen birth rate in 2021: 26.5 percent.] Arkansas is very anti-abortion. It’s very evangelical. Depending on how questions about abortions are asked, a majority of people here often favor making it illegal in most circumstances. Even exceptions to save the mother’s life usually mean the mother has to be actively dying in the emergency room before a doctor is legally allowed to give an abortion. And, as I mention in my book, the maternal mortality rate in Arkansas was already 50 percent higher than the national average.
Abortion was hard to get here even before the overturning of Roe. The closest clinic was ninety minutes away, in Little Rock, and that was the only abortion clinic operating in the state. If you couldn’t go there, usually you had to find a doctor willing to prescribe abortion medication, but I don’t know how easy that was, since it can be hard to get in to see a provider in a timely manner. Or you might’ve had trouble getting the morning-after pill. Now, people will have to travel even farther. The closest drive would be Illinois for a lot of Arkansans.
As for what that means, studies show how dangerous lack of access to abortion will be for maternal health. Looking at the longer term, when young girls have to become mothers, it has all kinds of effects on their lives that are hard to list.
Kelly: Is birth control readily available in rural Arkansas?
Potts: When I was a kid it wasn’t generally available or talked about, so it was hard for girls to get condoms, and to get on birth control if their moms objected. The girls that I grew up with had children fairly young and then they had tubal ligations. The Guttmacher Institute’s website mentions that tubal ligation is a common form of birth control for women in low-income communities. I imagine that’s because if you’re in the hospital already, for childbirth, it’s easy to ask the doctor to do the surgery for you. But to get birth control or an IUD, you’d need to see an OB-GYN—and there aren’t many here in my small town. A lot of people have to go at least an hour away to find one. A lot of women wait until they have a problem to seek help from a doctor in the first place.
Studies show how dangerous lack of access to abortion will be for maternal health … when young girls have to become mothers, it has all kinds of effects on their lives that are hard to list.
Kelly: Your book makes the case that having children young is one way the cycle of poverty replicates itself. Are there any sex education public health programs in rural America that give girls the tools to have safe sex without unplanned pregnancies?
Potts: Not that I’ve seen. In Arkansas, curriculum is up to individual schools. The Arkansas Democrat-Gazette conducted a survey in 2017 and found that nearly 85 percent of Arkansas’ 262 public school districts teach some form of abstinence, and that 34 districts didn’t teach any kind of sex education.
Kelly: When it comes to health care, how is rural America different from the rest of America?
Potts: For a lot of rural America, there isn’t a major hospital nearby. [A 2022 study found that rural residents typically travel five times further, more than twenty miles, to access hospitals compared to urban dwellers. The distance puts people suffering from acute emergencies like heart attack or stroke at greater risk of death.]
Not having a hospital nearby is a problem not only in an emergency. It means there aren’t a lot of doctors in the area, because they tend to work around hospitals. In my town [Clinton, Arkansas] we actually have a hospital, but for specialist care, people have to go farther away.
[The U.S. Government Accountability Office found more than half of rural counties lacked hospital-based obstetric services in 2018. By 2030, only about 50 percent of the demand for OB-GYNs in rural areas is expected to be met.]
That means [finding] health care takes a lot of time. You have to find a place that can treat you. If you have a long-term illness like cancer, there’s a good chance you have to drive an hour or ninety minutes. That’s a day when you can’t go to work.
The lack of options here means also that if you have a bad experience at one doctor’s office, you can’t go elsewhere.
Kelly: We saw during COVID-19 that rural America doesn’t seem to have a lot of faith in public health. How can experts encourage rural Americans to trust in public health more?
Potts: A Boston University sociologist, Matthew Motta, was at Oklahoma State University when he did a study about vaccine hesitancy. He found that a trusted actor who meets people where they are and explains what viruses are and what they do can overcome vaccine hesitancy. But it really takes an on-the-ground effort. You have to explain why this medicine or vaccine will be better than nothing. There is a general suspicion of anything that doesn’t seem like common sense, going back a long time. Knowledge that you get from personal experience is considered more trustworthy.
Book cover: Courtesy of Random House



