Ideas
AI is already tracking the next pandemic
For a motley collection of artificial intelligence researchers and startups, the end of the COVID-19 pandemic is just the beginning. The pandemic provided would-be entrepreneurs an opportunity to prove that artificial intelligence technology can help flag emerging illnesses before they turn into full-fledged epidemics.
While researchers have been experimenting with the technology for some time, COVID-19 created a surge of interest. BlueDot, an outbreak intelligence startup based in Toronto, says its customer base has grown by 475 percent surge since 2020 when it sent an alert to clients about an emerging illness in Wuhan five days before the World Health Organization announced it was tracking a “cluster of pneumonia cases” in the area. The company’s founder and CEO, Kamran Khan, says it has added vaccine manufacturers, as well as government and private security companies, to its customer list.
At Boston Children’s Hospital, officials started using AI to support capacity planning after the pandemic started, says John Brownstein, the hospital’s innovation officer. And Epiwatch, an AI epidemic surveillance service based at UNSW Australia, recently received a more than $5 million grant from Vitalik Buterin, the co-founder of the cryptocurrency Ethereum.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
“Traditional disease surveillance is done by health departments and will collect reports or notifications from hospitals, primary health care, and from laboratories,” explains Epiwatch’s founder, Raina MacIntyre. MacIntyre is also a public health physician and epidemiologist at UNSW Sydney. “By the time things land on the desk of a health department, usually the epidemic has already spread.”
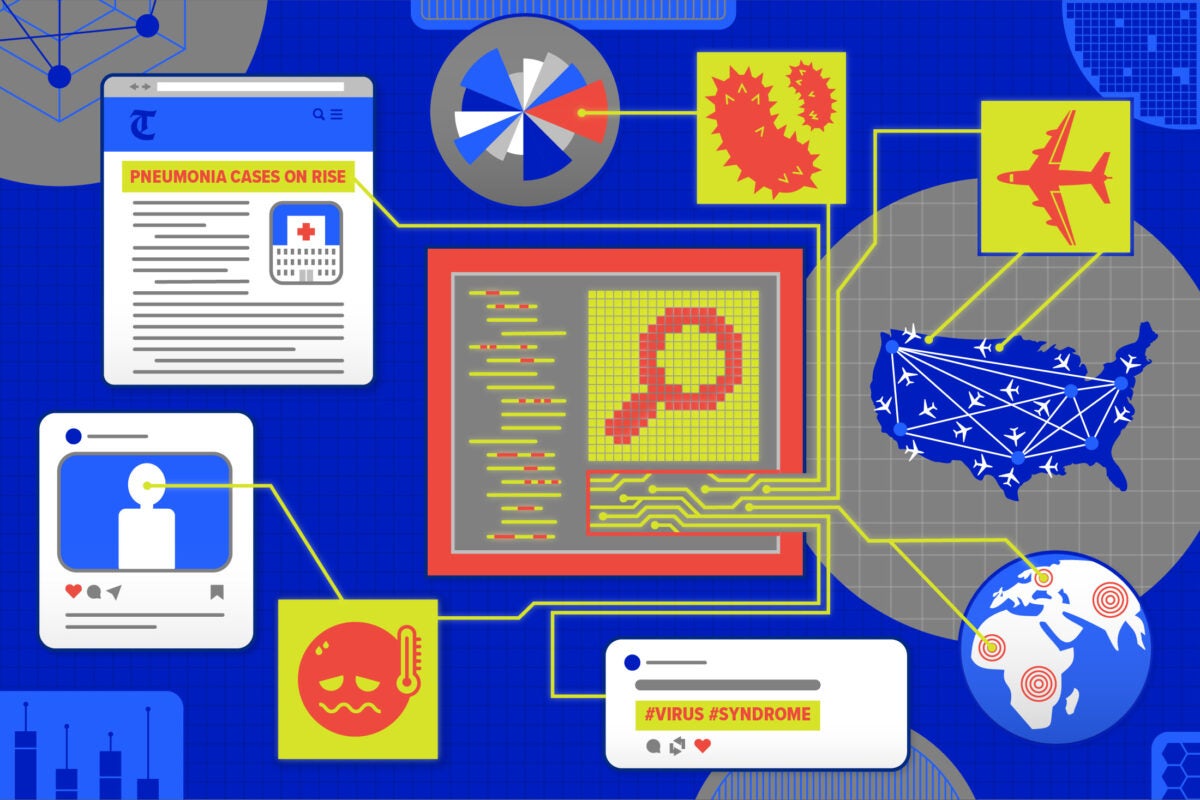
Epidemic surveillance AI usually involves algorithms that mine through sources of data—news reports, social media posts, and flight data—that aren’t traditionally used in disease surveillance. AI models can automatically scour this data, looking for patterns and abnormalities that public health authorities might not otherwise be aware of. For example, Epiwatch uses an AI technology called natural language processing that scrapes the web for terminology that could be associated with the emergence of a new illness, like “syndrome” and “pneumonia.”
McIntyre says that while AI can’t entirely replace health department epidemic monitoring based on lab tests and reports from healthcare institutions, companies like Epiwatch can still provide critical early warning data to officials— and give them a hint of where to look for a potential outbreak.
“It’s always about ‘garbage in, garbage out,’ and understanding the data that you’re feeding into these systems so that you can fully understand where the biases exist.”
John Brownstein, chief innovation officer, Boston Children’s Hospital
Critically, these AI systems weren’t just built to track COVID-19. At Boston Children’s Hospital, researchers have run a “Health Map” for more than a decade, says Brownstein. An earlier version of the software was able to flag one of the first signs of H1N1 in Mexico back in 2009. Epiwatch, meanwhile, was inspired by the World Health Organization’s slow reaction to the emergence of Ebola in West Africa in 2014.
Now AI researchers like Rachel Lowe, ICREA Professor at the Barcelona Supercomputing Center and the London School of Hygiene and Tropical Medicine, are looking to design systems that can factor in the impacts of climate change on disease spread.
“Let’s say that we have a particularly warm season and a particularly wet season, then our model might tell us that there is a high-risk thing in a particular place so we can predict an 80 percent chance of having a dengue epidemic in this place, given this combination of climate conditions,” Lowe said.
The system was used to forecast the potential spread of dengue ahead of the 2014 World Cup in Brazil, and Lowe also helped develop a dengue early warning tool that’s now being used in Vietnam.
Despite growing interest in this type of artificial intelligence, the technology does have significant limitations. For starters, these systems require an enormous amount of data. Building one of these models requires extensive computational power and cloud computing resources. Often, human analysts are still needed to review the findings that AI produces. These systems—like other forms of AI—can also incorporate bias.
“It’s always about ‘garbage in, garbage out,’ and understanding the data that you’re feeding into these systems so that you can fully understand where the biases exist,” explains Brownstein. “We know, for instance, with some of our tools, that, as much as we try to broaden out languages, we’re going to have a real bias in terms of geographic representation globally, based on where there are media sources and data.”
Another challenge with AI-based pandemic modeling is the technology’s “black box.” While AI can be used to make predictions, it is sometimes impossible to understand why a system ultimately makes the forecast that it does.
Still, researchers and startup founders alike hope that AI, even with its constraints, can serve as an early warning system and helping hand to public health officials looking to stop the spread of an illness. At the very least, the technology provides an easy way of flagging social media posts and online articles that reveal where people are starting to get sick— digital low-hanging fruit that could potentially save lives.
Due to incorrect information supplied by the company, an earlier version of this story said BlueDot had reported an emerging pneumonia cluster in Wuhan, China nine days before the World Health Organization. The actual timing was five days before.