Opinion
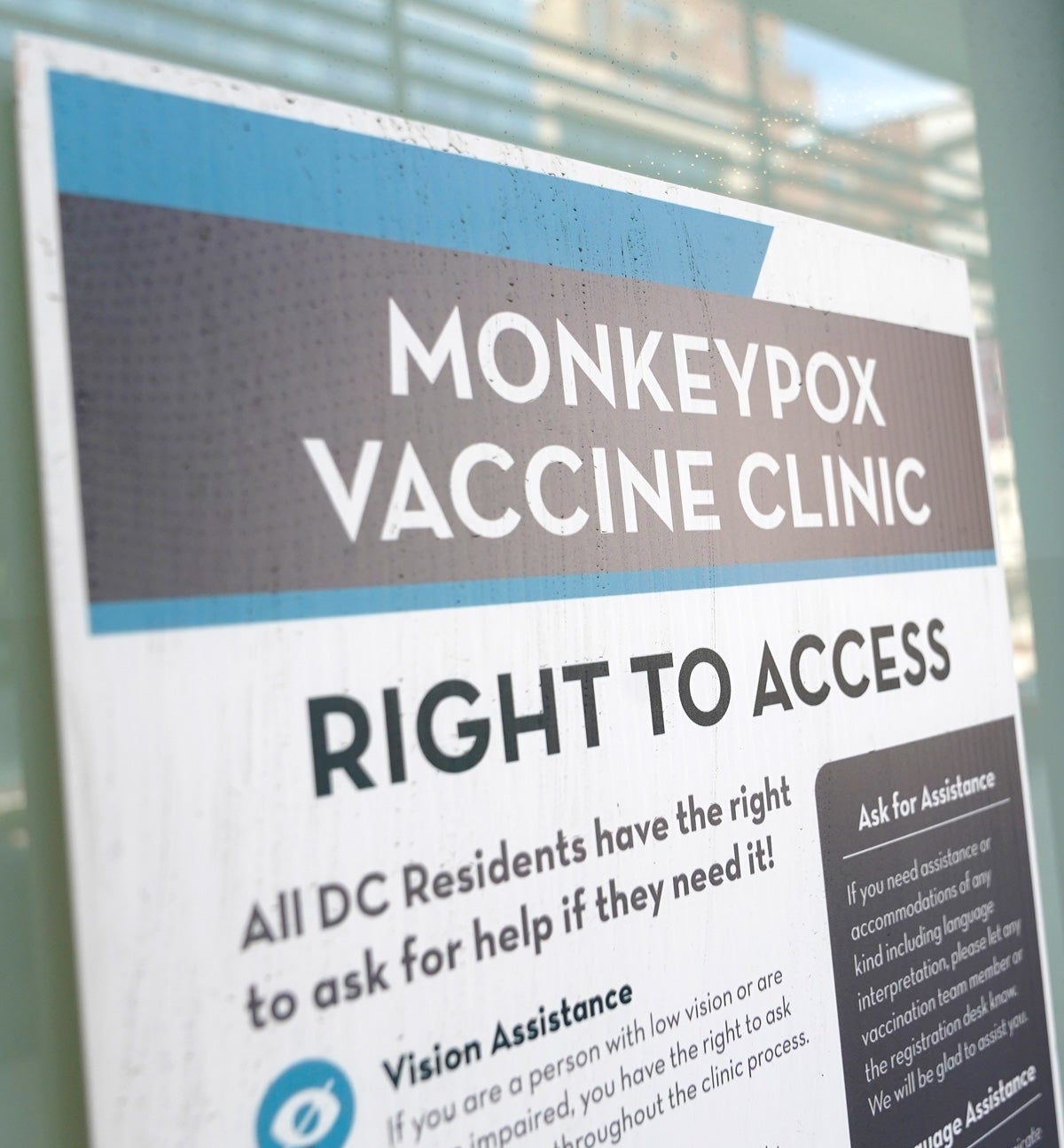
An open letter to the Biden administration on monkeypox
To: Robert Fenton, White House National Monkeypox Response Coordinator, and Dr. Demetre Daskalakis, White House National Monkeypox Response Deputy Coordinator:
We write as a group of scholars, activists, and members of the queer and trans community calling on the Biden administration to implement a comprehensive response to the outbreak of monkeypox (MPX).
Over the past four months, we have watched MPX infect members of our community. As of August 5, there have been 7,510 confirmed cases of MPX in the U.S. and 28,220 confirmed cases globally. Despite warnings in Europe and other regions of the world, the Biden administration ignored our early calls for testing and missed its chance to stop infections in the U.S.
The Biden administration finally declared MPX a public health emergency, appointing you to lead the White House’s national response. While this is long overdue, we welcome you and your team, and we want you to know it is not too late to stop the spread of MPX. To do so, we need a comprehensive response that puts affected communities first and makes prevention, health education, testing, vaccines, and treatment widely available both in the U.S. and abroad.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
Queer and trans communities face ongoing racism, homophobia, and transphobia. These and other social, structural, and historical disadvantages — like medical gaslighting by health care providers — place them at much greater risk of infection with MPX. Stigma affects access to and quality of care, causing significantly worse health outcomes, including HIV and other chronic diseases. MPX may infect queer and trans communities first, but these communities will not be the last. We demand action now.
The Biden administration’s response to MPX must engage affected communities, especially Black, Indigenous, Latinx, Asian and Pacific Islander, queer and trans communities; sex workers; people living with HIV; people who inject drugs; and people experiencing homelessness in rural and urban settings. As we have said before, it is critical to include those most at risk in the response and equip them with the information and resources they need to keep themselves and our community safe.
We propose 11 policy solutions — identified by the queer and trans community, scholars, and activists — that the Biden administration should implement to center health equity and improve its response to MPX:
- Include Black, Indigenous, Latinx, Asian and Pacific Islander, queer and trans communities in positions of leadership to oversee the response.
- Promote free testing, vaccination, and condoms at community venues, such as bars and clubs frequented by queer and trans communities.
- Scale procurement and partnerships with other manufacturers to increase capacity, production, and access to vaccines and treatment, with provisions for treatment outside of the current investigational new drug protocol.
- Partner with private insurance companies and the Centers for Medicare & Medicaid Services to codify health insurance coverage for MPX-related prevention, testing, and treatment.
- Increase resources to support staff in front-line agencies (e.g. city sexual health clinics and LGBTQ health centers) to diagnose the increasing number of cases and to scale up vaccine delivery as supplies become more plentiful.
- Regulate the adoption of work and travel protections for those required to quarantine because of MPX infection, including mental health support and direct financial assistance to mitigate the psychosocial and economic impacts of isolation.
- Develop a surveillance system that collects and provides transparent data on MPX by race, ethnicity, gender identity, and sexual orientation to hone local response efforts in testing, vaccination, and treatment.
- Support rapid research for tests that can be taken at home to detect MPX early on, prior to the development of painful sores. It has taken providers about four hours to complete a 16-step process per patient to test for MPX and prescribe TPOXX. We must also replicate “test and treat” models of care from the response to HIV and COVID-19 to quickly prescribe treatment after a patient tests positive for MPX.
- Educate providers, lab workers, and queer and trans communities about MPX through the launch of innovative marketing and communications campaigns, with support from community health workers. These campaigns must not stigmatize LGBTQ+ communities: we should communicate with the public that MPX can infect anyone, regardless of sexual orientation and gender identity. Additionally, as the epidemic spreads beyond urban jurisdictions, education will be imperative for rural health departments to identify cases early.
- Invest resources for the global response in regions where MPX is already endemic, like in west and central Africa.
- Fund future research in clinical medicine and public health to better understand MPX and other emerging infectious diseases so we can better inform evidence-based policies for emergency response.
By implementing these 11 policy solutions, we anticipate a comprehensive response that is not only focused on containment in the U.S. but also addresses MPX around the world. We are optimistic that your experiences, particularly Dr. Daskalakis’s long history in HIV-related advocacy, will lead to the implementation of these policies.
Sincerely,
Jennifer Barnes-Balenciaga, Co-Investigator, RESPND-MI; Director, Crystal La’Beija Organizing Fellowship
Sean Cahill, PhD; Director of Health Policy, The Fenway Institute
Pedro Botti Carneiro, MPH; Co-Investigator, RESPND-MI
Tom Carpino, MPH; Co-Investigator, RESPND-MI; Doctoral student, Johns Hopkins Bloomberg School of Public Health
Nicholas Diamond, MPH; Co-Investigator, RESPND-MI
Zhiting (Jack) Feng, MHS; Research Data Manager, MACS (Multicenter AIDS Cohort Study)/WIHS (Women’s Interagency HIV Study) Combined Cohort Study (MWCCS), Johns Hopkins Bloomberg School of Public Health
William C. Goedel, PhD; Reference Group, RESPND-MI; Assistant Professor, Brown University School of Public Health
Ian W. Holloway, PhD, LCSW, MPH; Reference Group, RESPND-MI; Director, UCLA Gay Sexuality and Social Policy Initiative
Lawrence C. Long, MCom, PhD; Reference Group, RESPND-MI; Research Assistant Professor, Boston University School of Public Health
Keletso Makofane, MPH, PhD; Principal Investigator, RESPND-MI; Health & Human Rights Fellow, Harvard University
Kenneth Mayer, MD; Reference Group, RESPND-MI; Co-Director, The Fenway Institute
Joseph Osmundson, PhD; Co-Investigator, RESPND-MI; Clinical Assistant Professor of Virology, New York University
Asa Radix, MD, PhD; Senior Director of Research and Education, Callen-Lorde Community Health Center
Grant Roth, MPH; Co-Investigator, RESPND-MI
Martez D. R. Smith, LMSW; Co-Investigator, RESPND-MI; Doctoral Candidate, University of Rochester School of Nursing
Nguyen K. Tran, MPH, PhD; Co-Investigator, RESPND-MI; Postdoctoral Scholar, the PRIDE Study, Stanford University School of Medicine
RESPND-MI – Rapid Epidemiologic Study of Prevalence, Networks, and Demographics of Monkeypox Infection – is a LGBTQ+ community-led survey of monkeypox symptoms and networks among queer and trans people in New York City.
This post was updated on Aug. 9 to match the language of the open letter as agreed to by all signatories.
Top photo: Patrick Semansky / AP Photo