Feature
Hard lessons on COVID-19 in the midst of hope
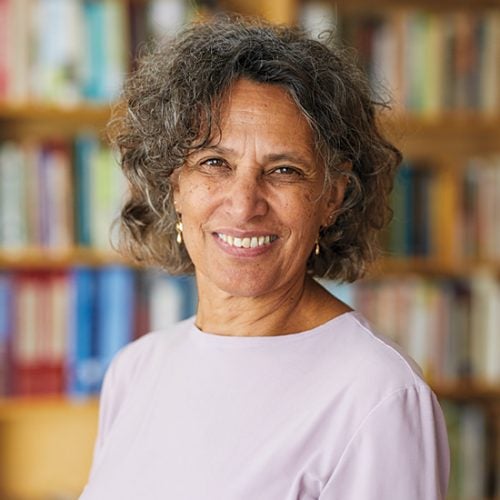
Enduring its second year of a devastating COVID-19 pandemic, the world faces a potential turning point in the struggle against a tiny virus that has killed millions, exposed and preyed upon deep social inequalities, wrecked economies, and put ordinary life on hold. There is now tremendous hope sparked by the record pace of vaccine development and the start of a massive, yet halting and unequal, inoculation effort. New COVID-19 infections are still alarmingly high and rife with proliferating viral variants that threaten to undo progress against the contagion. Contributing writer Chris Berdik spoke with a group of leading researchers at the Harvard T.H. Chan School of Public Health about vaccines, variants, and how we can best prepare for the next potential pandemic.
Q: COVID-19 is the biggest global scientific and public health challenge in living memory. In broad strokes, how do you rate the battle against the pandemic one year in?
HOWARD KOH: When the first COVID-19 cases were documented in January 2020, who would have predicted that the pandemic would extend well into a second year and cause well over half a million deaths in this country? History tells us that the 1918 pandemic killed 675,000 Americans. We are now within striking range of that terrible figure from a century ago, despite all the advances we’ve made since in medicine and public health. Though there’s been heroic work by medical and public health professionals everywhere and a decline in cases and hospitalizations recently, this pandemic remains a public health catastrophe that holds so many lessons for generations to come.
MARY T. BASSETT: Certainly, it was possible to predict that the United States would fare very poorly. In March of last year, my colleague Natalia Linos and I wrote a piece in the Washington Post that said that many of the features of U.S. society—escalating income inequality, growing and sustained racial-ethnic differences in disease experience and mortality, the growing precarity of work with the emergence of the gig economy, and the loss of labor and environmental protections—have made us more vulnerable to a pandemic than other wealthy countries.
Additionally, the U.S. has always underinvested in public health infrastructure compared to other wealthy countries, yet the share of the budget going to public health keeps declining, and Trump cut investments in pandemic preparedness. All these factors made it more likely that people would be exposed. While the vaccine brings great promise, we cannot forget what made the U.S. so vulnerable in the first place.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
MARC LIPSITCH: I think the biggest highlight is clearly the vaccine. It’s a triumph in the sense that we did it faster even than people thought we could do in April 2020, and it’s a triumph in the sense that five years ago, we would have been nowhere near this prepared. The two biggest actors that I can think of to credit for that are the National Institutes of Health [NIH] and the Coalition for Epidemic Preparedness Innovations [CEPI], which did not exist five or six years ago.
CEPI was set up with the Norwegian government and some other early sup-porters, and has offices in London and Washington. They started giving out money to build platforms for vaccines, including adenovirus platforms, and for work specifically on coronavirus vaccines, among a few others. Coronavirus was a lucky bet in a sense, but it was informed luck.
SARAH FORTUNE: As a bench scientist, I have to say that I think one of the things that has gone exceedingly well has been the scientific effort to understand the virus and the vaccines. While it’s easy to focus on domestic successes, it has been a global effort, with the first Chinese identification of the virus and then the publication of the viral genome, which enabled all of the diagnostic and therapeutic tools that we have built.
It has just been so sobering to see how a pandemic reveals all the cracks in society. If there were fault lines, the pandemic has made them exceptionally clear. Those are fault lines in international relationships, fault lines in domestic policy, fault lines in health equity.
“If we don’t help eradicate COVID-19 globally, all we do is ensure that this disease will recur regularly in the United States.”
Howard Koh, Harvey V. Fineberg Professor of the Practice of Public Health Leadership
Q: The urgency of fighting the pandemic has pushed more sharing of findings before peer review, a condensing of clinical trials, and a renewed focus on coordinating research efforts for speedier progress. What aspects of these shifts can and should be retained without endangering scientific rigor?
MARCIA CASTRO: We saw collaborations among groups that previously didn’t collaborate. In Boston, we had all the hospitals collaborating. That never happened before, and that’s a positive development. And I hope that attitude remains, because we can work and disseminate knowledge much better and much faster by joining efforts. For anything in public health, really, but particularly in the middle of a pandemic, you need different kinds of knowledge. To respond to the pandemic, we need more than epidemiologists, immunologists, and virologists. We need to bring the social sciences. It has to be a multidisciplinary and joint effort.
FORTUNE: There’s been a huge shift of resources into this scientific endeavor. There has been an emphasis not just on speed but on tangible progress. The willingness of the journals to get papers out, rather than turn them over and over again in review, promotes a sense that science is a conversation, and we need to move that conversation forward. Those are important lessons from this pandemic.
Now, whether or not there is going to be an appetite for the kinds of resources that have enabled multiple parallel clinical trials, for example, is unclear. I work on tuberculosis, which was only this year surpassed by COVID-19 as the leading infectious cause of death. But there is no sense of urgency with TB, no sense of alarm, no sense of moral outrage. And that is reflected in the fact that the resources devoted to TB are minuscule compared to the resources devoted to COVID-19. So, certainly, the jettisoning of the unhelpful barriers to progress should become the norm, but I don’t know if we can expect greater concentration of resources in other scientific endeavors to drive light-speed progress as we move forward.
Q: Scores of COVID-19 vaccines are in various stages of development and approval, but we are also now becoming keenly aware of the additional steps required to get vaccines distributed and into people’s arms—in the U.S. and around the world. What have we learned about the challenges of vaccine development and distribution in the past year?
LIPSITCH: At every level, from comparing countries to comparing deciles of income in a country, the rich get richer. The wealthiest people are the most likely to get access to the vaccines, and they are also the ones who can socially distance more easily, who can work from home, and who can minimize their risk in other ways.
Still, I’m sympathetic with the people trying to make distribution decisions, because I’ve been on the Massachusetts committee that advises the governor on these things. Take an issue like vaccine tourism. Every jurisdiction should want to vaccinate its own people rather than people from outside. On the other hand, what are the solutions? You could ask for a driver’s license, but if you ask for driver’s licenses, you keep certain groups of people away, many of whom are most in need of a vaccine. There’s no perfect solution, especially when you’re starting with a completely inadequate health care system for a large fraction of the population, which has consequences for all of us.
FORTUNE: I think there are a couple of interesting lessons. The first is that investment in innovation pays off. We tend to declare the Pfizer and the Moderna vaccines as miracles of modern science, because we went from no vaccine to a vaccine in nine months with these new platforms. But in fact, the platforms exist because of nearly two decades of investment after the bioterrorism threats in the early 2000s that led to a sense that we needed rapidly deployable vaccines.
The second point is, in fact, there is no single solution. It’s important to have multiple shots on goal and to recognize the value in different solutions, because vaccines are only effective if there are vaccines in people. That is the finish line, not efficacy in a clinical trial.
And we’re not done, right? We have some real challenges coming down the pike in the virus variants. These smaller academic biotechs are pursuing highly innovative vaccines that are going to target different aspects of the virus that could be important as we plan for the potential recurrence of immune-resistant variants.
Illustration: Jake Olimb / iStock
Q: One huge story to emerge during this pandemic is its unequal impacts and how COVID-19 both revealed and widened vast structural inequalities in the U.S. From a public health perspective, what should the top priorities be to address these inequities?
BASSETT: These inequities that have emerged in the last 40 years can be reversed, but it requires political will, principally. We have to address the living conditions of working people and the escalating misery of poor people and undocumented people and emphasize that these inequities pose a risk to everyone. It seems very likely that this is not the last novel virus that we’ll see, and we can’t rely on a vaccine to protect us from this pandemic or future pandemics.
We also need to address the fact that we continue to have millions of people who lack health insurance coverage. I am a long-standing advocate for single-payer health care. We are seeing what a privatized, profit-driven commercial system can do in terms of fragmented delivery. The U.K.’s national health care system, for example, has been able to roll out the vaccine more effectively than the U.S.
But there are interim measures we can take. For instance, there are still states that have declined federal funding for the expansion of Medicaid, which is the principal way people got extended health insurance coverage under the Affordable Care Act. And everything should be done to prevail on those states to accept Medicaid expansion.
LIPSITCH: I think there are two big priorities: The first is giving everybody adequate access to health care, preventive care, and a primary care provider, as well as a nonbankrupting way to use health services when needed. The second would be to fix our information systems. They are catastrophic. Understanding the burden of disease is unbelievably fragmented.
As a point of comparison, Israel has been able to deliver vaccinations much more rapidly than most countries. That’s because everybody in the country is a member of one of four HMOs that know everything about those people’s health. Early on in the pandemic, they could develop risk scores by analyzing their databases and figuring out who was getting infected and who was getting hospitalized and target messaging to people individually about what they needed to do to protect themselves.
Now that vaccinations are underway, they’re able to know what day every person got their first dose and their second dose. For every person in the country, they know if they previously had COVID-19, in which case they’re not recommended to get vaccinated, or if they are in a high-risk group, in which case they’re prioritized for vaccine.
Q: What can be done to supply vaccines to developing countries? And what about the infrastructure and logistics involved in storing these vaccines and getting them into people’s arms?
CASTRO: The logistics is a challenge. Some places in Africa or even in Brazil are remote. You need hours to get there. You need to take boats. You have no paved roads.
Now, the issue is, the more vaccines you have in your portfolio, the better you are, because in capital cities—in any part of the world—you can deploy those vaccines that require cold storage, and then, in the more isolated places, you use the others that don’t need special freezers.
BASSETT: The U.S. has rejoined the World Health Organization [WHO] and has joined COVAX [COVID-19 Vaccines Global Access], so those are good moves. But when we talk about the inequities within the United States, they really seem minor compared to the inequities between nations. I lived and worked in Zimbabwe for many years. And just a week ago, I lost—the country lost, their families lost—two leading medical researchers to COVID-19. It’s just a tragic situation.
Tedros Adhanom Ghebreyesus, director general of the WHO, has been really eloquent about the fact that the world faces a moral challenge. And I hope the United States, as it seeks to regain its role globally, will rise to this challenge. There are many vaccines under development. But the United States, so far, has led the pack in developing highly effective vaccines, and people are raising questions about licensing the technology to other producers. These are conversations that need to be had.
KOH: If we don’t help eradicate COVID-19 globally, all we do is ensure that this disease will recur regularly in the United States. So being a leader and partner in the global community means the U.S. needs to commit to this work as part of our future self-interest. And if every nation adopts that attitude and commitment, we can move forward. Fortunately, President Biden, on his first day, announced his decision to rejoin the WHO and the COVAX effort that Mary noted. And that was a huge signal to the country and the world.
“We don’t really have good genomic surveillance in most countries. So, when new variants emerge, we don’t track them soon enough.”
Marcia Castro, Andelot Professor of Demography and chair of the Department of Global Health and Population
Q: How big a problem is vaccine hesitancy and misinformation, and what more can or should be done to overcome it?
CASTRO: It’s a global problem. The amount of misinformation circulating that looks legit is unbelievable. And it circulates across all social media channels and in WhatsApp. In Brazil, the president said that he’s not going to get vaccinated and made comments about how he’s not to blame if the vaccine turns you into an alligator. That is not the kind of behavior one would expect from the leader of a nation. Instead, we should be having massive communication campaigns bringing the message that vaccines are safe and effective.
So, in Brazil, we created a website. It’s the Alligator Tracker. And it gives the number of people vaccinated in the world and the number of people vaccinated in Brazil. It also shows how many people turned into alligators; I’m happy to say it’s still zero.
LIPSITCH: I think the numbers of even health care workers who are saying they don’t want a vaccine yet are indicative that it is a problem. I don’t know how much of that is misinformation. I think there’s a lot of mistrust built up, over decades, toward the health system among some groups of people.
There was a large amount of garbage that came out of the highest levels of government in the first year of the pandemic, and I’m very sympathetic to people who don’t trust what they hear. I think we need to fix that trust or improve that trust, but it’s going to take some time.
BASSETT: That said, there also is a concern that this mistrust is not based on myth but based on lived experience and history of mistreatment by the medical establishment of people in this country who are classified as Black. There’s been a problem with trustworthiness, and there’s a need to prove trustworthiness.
Unfortunately, it seems to me that the vaccination rollout is not helping with trustworthiness. It’s extremely difficult for people to figure out how to schedule a vaccination. And the WHO some time ago, in talking about how to boost vaccinations, talked about tackling complacency, confidence, and convenience. And the convenience factor has not been successfully addressed yet.
Communities of color have fewer vaccination sites—and the data already show large racial disparities in who’s been vaccinated. The likelihood of being vaccinated can be two- to threefold higher in whites than among Blacks, despite their higher disease burden and higher mortality burden. It should not be difficult to get vaccinated. And I think that if we can solve the convenience issue, it will be a lot easier to tackle the other types of barriers, the individual barriers to seeking vaccines.
Q: How worried should we be about the emerging viral variants?
FORTUNE: Am I allowed to say terrified? Any interaction between a pathogen and its human host is fundamentally an evolutionary arms race. We have not fully come to terms with how that arms race plays out and what aspects of our policies give the pathogen the advantage. So, we have these fabulous vaccines, many of which are pretty narrowly focused on one portion of the virus. We know that across the world there’s just a huge amount of viral diversity because we let this virus get out of control.
All of that viral diversity is going to come right up against the immune pressure of our previously infected and vaccinated populations. Most of that immune pressure is going to be sufficient to stop the spread of the virus. But rare events, rare viruses that break through that immune pressure, exist in the population, and, by the nature of evolution, they will then be able to propagate through a vaccinated and previously infected population. If we don’t get our heads around that, we are in for cyclic rounds of viral transmission. I think that means we’re going to be dealing with some variant of this coronavirus for a long time.
CASTRO: It is not by chance that some of the variants are emerging in the U.K., in South Africa, in Brazil. These countries have very high transmission. If you have a large fraction of the population that has been infected already, the virus will try to find new ways to evolve.
In the city of Manaus, in Brazil, we estimated that 76 percent of Manaus’ population had been infected by October 2020. A new variant of concern, called P.1, emerged, most likely in November. This variant is about 1.4 to 2.2 times more transmissible than other lineages and can evade protective immunity from a previous infection. Last January, Manaus witnessed one of the most tragic scenarios of overwhelmed hospital capacity, not only running out of hospital beds but also oxygen.
The fear is that you could have another variant that is even more rare and could be more lethal. And that would be probably the worst-case scenario. I’m really concerned. We don’t really have good genomic surveillance in most countries. So, when new variants emerge, we don’t track them soon enough.
LIPSITCH: It is bad news. The question is, how bad? I think it’s pretty clear that the existing vaccines work against the B.1.1.7 U.K. variant. I think it’s fairly clear that the current vaccines will provide some protection, especially against severe outcomes, for the B.1.351 variant, the South African variant. I’m not aware of much data on the P.1 variant. But the variants all do have an overlapping set of mutations. So, I think there’s some reason to try to extrapolate. I think it does add pressure to get vaccines out quickly, not only to save lives, but just to get ahead of the spread of these variants, at least until we can create new vaccine strains.
“Many people in this pandemic died because their local health care system was underfunded, undervalued, and didn’t have the resources to take care of them. That’s not a scientific agenda. That’s a health equity agenda.”
Sarah Fortune, John LaPorte Given Professor of Immunology and Infectious Diseases and chair of the Department of Immunology and Infectious Diseases.
Q: This magazine will be published on the cusp of summer. What are your optimistic and pessimistic forecasts for where we’ll be then in the battle against this pandemic? And what are the main drivers for your pessimistic or optimistic scenario becoming our summer reality?
FORTUNE: In my optimistic scenario, people have come to understand that the restrictions of masks and other risk-mitigation strategies can easily be incorporated into daily life, combined with more robust vaccine coverage, so we can dramatically reduce viral transmission in our communities, reduce hospitalizations, and reduce deaths. That would allow so many aspects of our normal societal functioning, things we love, to come back—restaurants, bars, gyms.
But even in my optimistic scenario, people are still cautious and thoughtful. People are still wearing masks. If people feel sick at all, they’re staying home and getting tested, even if they’ve been vaccinated. They’re really careful, both for their own health, for their family’s health, and for their community’s health. If I’m really optimistic, we will have invested even more in the public health infrastructure that is sort of quietly helping us maintain the gains that we have achieved.
Pessimistic is we realize that some of these viral variants that are circulating actually have substantial ability to infect people who have already been vaccinated or previously infected. So, our assumptions about vaccine-mediated immunity were overly rosy, and we’re scrambling to come up with second-generation vaccines to boost people when we haven’t even fully vaccinated the population with first-generation vaccines.
KOH: Optimistically, by summer, the COVID-19 vaccines will be readily available for everybody. That’s something we all eagerly anticipate. If acceptance continues to rise, we hope that we can reach herd immunity sometime in late summer or early fall.
And then, hopefully, we could return to some sense of normalcy, although life will never be exactly what it was before COVID-19.But variants are not the only challenge. Vaccine hesitancy could also remain a major obstacle. And then, until we reach herd immunity, we need to emphasize that vaccination complements broader prevention measures like continued mask usage and social distancing and other recommendations. Can we unify and implement all these measures as a nation going forward? I sure hope so.
Q: There is no shortage of priorities to better prepare for the next potential pandemic. What should be at the top of that list?
LIPSITCH: First, we should take the CEPI model for developing vaccines and replicate it for diagnostics and therapeutics, so that we have the same ability to develop treatments quickly if needed. The second thing I would prioritize would be broadly revitalizing public health information systems.
By that, I mean everything from how do you get a representative sample of the population and learn something about them all the way up to how do you aggregate information about who’s gotten vaccines and who’s gotten sick and who hasn’t? We shouldn’t have to rely on Johns Hopkins or The Atlantic to be the center of the nation’s biostatistics. That’s the job of a national government.
Number three, and maybe actually number one in importance, is building a health care system that is efficient and equitable.
FORTUNE: Yeah, I think number one on my list is the need to address equity in our health care system. Many people in this pandemic died because their local health care system was underfunded, undervalued, and didn’t have the resources to take care of them. That’s not a scientific agenda. That’s a health equity agenda. I think that we need to fix that, even if not flogged by the threat of the next great pandemic.
In preparing for the next pandemic, we need to continue to invest broadly in basic science research, recognizing we don’t know where the next pandemic is going to emerge.
Just to give you a sense of how lucky we got: In 2019, prior to the coronavirus pandemic, the NIH had maybe 20 grants in coronavirus research, compared to hundreds and hundreds of grants in HIV, let’s say. So, I think, as a scientific community, we had made a decision about where the next great threat was going to be, and we were myopic in terms of where we put our resources. Then, continue the investment that we made in vaccine platforms.
CASTRO: We need an international coalition that can work together to create a surveillance network that can identify new pathogens when they emerge. The network should integrate epidemiological and genomic surveillance, so both known and emerging pathogens can be monitored and actions taken to mitigate outbreaks.
That’s our best bet in trying to identify new pathogens as they emerge. That’s going to demand equipping some countries both with physical infrastructure and capacity building of personnel. It has to be spearheaded by the countries that have the technology to do this and the resources to help the countries that don’t. Whether it’s the World Health Organization that pushes this effort or another international institution, it needs to happen.
And honestly, this is a terrific investment. If you think about how much it would cost to create a system like this—training personnel, putting in equipment and the technology of a well-designed network—that’s peanuts compared to all the money that we are spending to fight this pandemic, and to all the lives lost.
KOH: I often point out that when prevention and public health work, absolutely nothing happens—except the miracle of a perfectly normal, healthy day. Prevention sounds easy, but it’s not. The catastrophe we’re enduring is because, as a society, we have never invested in prevention and public health the way we should.
Once we get this pandemic behind us, we must reinvest in public health and revitalize this lifesaving field. Our nation must commit to providing the resources and infrastructure and personnel that the field has long needed and deserves. But we will have to see if that’s going to happen. Public health has been overlooked and underappreciated for far too long.
Also, this catastrophe is a fast pandemic fueled by slower pandemics of chronic preventable conditions such as obesity, heart disease, and lung disease. The health inequities throughout all these areas have been long-standing and unacceptable. So, are we going to take a systematic approach to all this and really make prevention come alive in the future? That’s the overriding question. If we don’t do so in a fundamental way soon, our global society risks enduring such suffering yet again. And we simply cannot allow that to happen.
Top illustration: Jake Olimb / iStock