Ideas
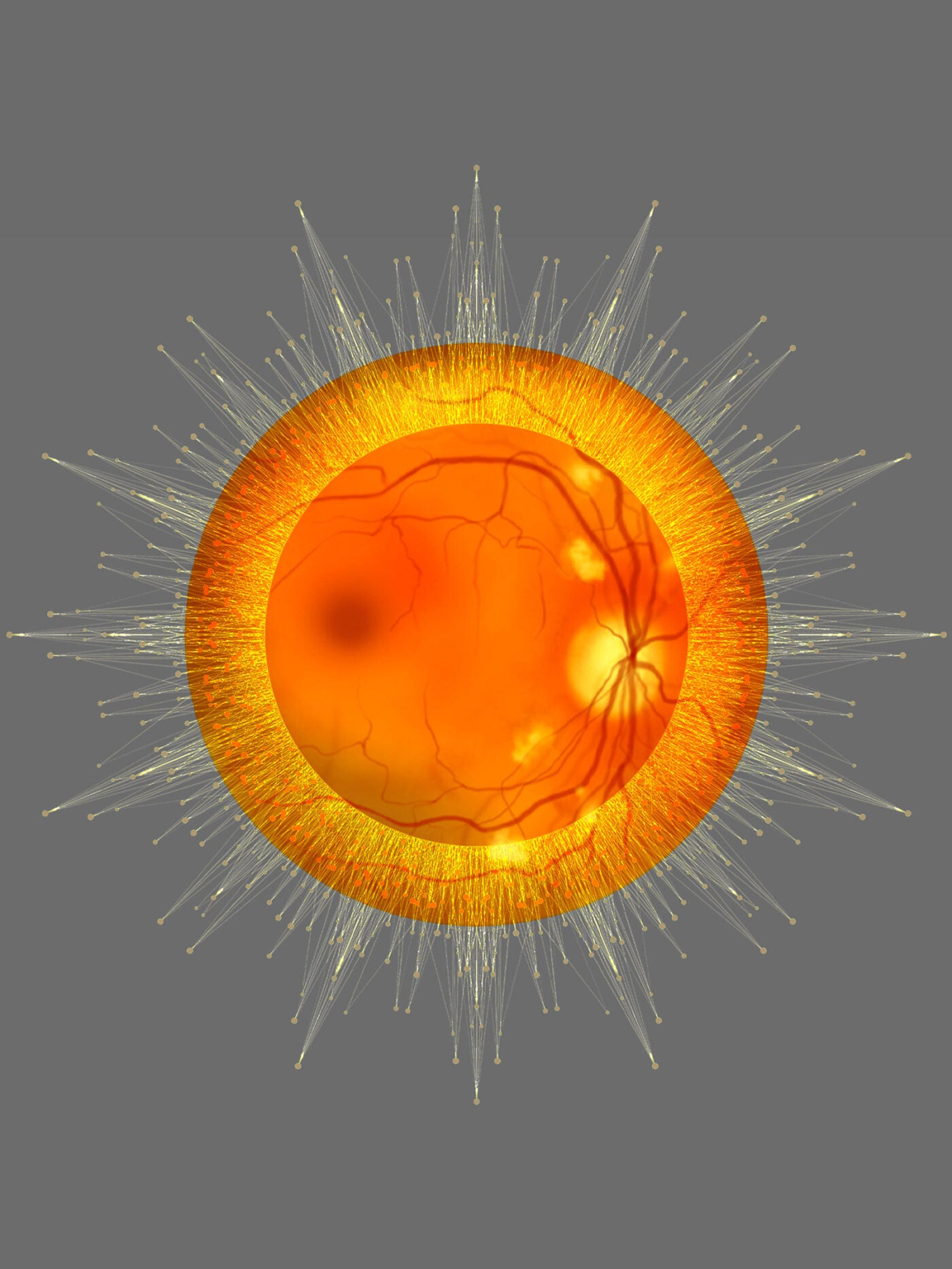
As AI-based eye exams prove their worth, lessons for future tech emerge
This article was originally published by KFF Health News.
Christian Espinoza, director of a Southern California drug-treatment provider, recently began employing a powerful new assistant: an artificial intelligence algorithm that can perform eye exams with pictures taken by a retinal camera. It makes quick diagnoses, without a doctor present.
His clinics, Tarzana Treatment Centers, are among the early adopters of an AI-based system that promises to dramatically expand screening for diabetic retinopathy, the leading cause of blindness among working-age adults and a threat to many of the estimated 38 million Americans with diabetes.
“It’s been a godsend for us,” said Espinoza, the organization’s director of clinic operations, citing the benefits of a quick and easy screening that can be administered with little training and delivers immediate results.
His patients like it, too. Joseph Smith, who has Type 2 diabetes, recalled the cumbersome task of taking the bus to an eye specialist, getting his eyes dilated, and then waiting a week for results. “It was horrible,” he said. “Now, it takes minutes.”
Sign up for Harvard Public Health
Delivered to your inbox weekly.
Amid all the buzz around artificial intelligence in health care, the eye-exam technology is emerging as one of the first proven use cases of AI-based diagnostics in a clinical setting. While the FDA has approved hundreds of AI medical devices, adoption has been slow as vendors navigate the regulatory process, insurance coverage, technical obstacles, equity concerns, and challenges of integrating them into provider systems.
The eye exams show that the AI’s ability to provide immediate results, as well as the cost savings and convenience of not needing to make an extra appointment, can have big benefits for both patients and providers. Of about 700 eye exams conducted during the past year at Espinoza’s clinics, nearly one-quarter detected retinopathy, and patients were referred to a specialist for further care.
Diabetic retinopathy results when high blood sugar harms blood vessels in the retina. While managing a patient’s diabetes can often prevent the disease—and there are treatments for more advanced stages—doctors say regular screenings are crucial for catching symptoms early. An estimated 9.6 million people in the U.S. have the disease.
The three companies with FDA-approved AI eye exams for diabetic retinopathy—Digital Diagnostics, based in Coralville, Iowa; Eyenuk of Woodland Hills, California; and Israeli software company AEYE Health—have sold systems to hundreds of practices nationwide. A few dozen companies have conducted research in the narrow field, and some have regulatory clearance in other countries, including tech giants like Google.
Digital Diagnostics, formerly Idx, received FDA approval for its system in 2018, following decades of research and a clinical trial involving 900 patients diagnosed with diabetes. It was the first fully autonomous AI system in any field of medicine, making its approval “a landmark moment in medical history,” said Aaron Lee, a retina specialist and an associate professor at the University of Washington.
The system, used by Tarzana Treatment Centers, can be operated by someone with a high school degree and a few hours of training, and it takes just a few minutes to produce a diagnosis, without any eye dilation most of the time, said John Bertrand, CEO of Digital Diagnostics.
The setup can be placed in any dimly lit room, and patients place their face on the chin and forehead rests and stare into the camera while a technician takes images of each eye.
The American Diabetes Association recommends that people with Type 2 diabetes get screened every one to two years, yet only about 60 percent of people living with diabetes get yearly eye exams, said Robert Gabbay, the ADA’s chief scientific and medical officer. The rates can be as low as 35 percent for people with diabetes age 21 or younger.
In swaths of the U.S., a shortage of optometrists and ophthalmologists can make appointments hard to schedule, sometimes booking for months out. Plus, the barriers of traveling to an additional appointment to get their eyes dilated—which means time off work or school and securing transportation—can be particularly tricky for low-income patients, who also have a higher risk of Type 2 diabetes.
“Ninety percent of our patients are blue-collar,” said Espinoza of his Southern California clinics, which largely serve minority populations. “They don’t eat if they don’t work.”
One potential downside of not having a doctor do the screening is that the algorithm solely looks for diabetic retinopathy, so it could miss other concerning diseases, like choroidal melanoma, Lee said. The algorithms also generally “err on the side of caution” and over-refer patients.
But the technology has shown another big benefit: Follow-up after a positive result is three times as likely with the AI system, according to a recent study by Stanford University.
That’s because of the “proximity of the message,” said David Myung, an associate professor of ophthalmology at the Byers Eye Institute at Stanford. When it’s delivered immediately, rather than weeks or even months later, it’s much more likely to be heard by the patient and acted upon.
Myung launched Stanford’s automated teleophthalmology program in 2020, originally focusing on telemedicine and then shifting to AI in its Bay Area clinics. That same year, the National Committee for Quality Assurance expanded its screening standard for diabetic retinopathy to include the AI systems.
Myung said it took about a year to sift through the Stanford health system’s cybersecurity and IT systems to integrate the new technology. There was also a learning curve, especially for taking quality photos that the AI can decipher, Myung said.
“Even with hitting our stride, there’s always something to improve,” he added.
The AI test has been bolstered by a reimbursement code from the Centers for Medicare & Medicaid Services, which can be difficult and time-consuming to obtain for breakthrough devices. But health care providers need that government approval to get reimbursement.
In 2021, CMS set the national payment rate for AI diabetic retinopathy screenings at $45.36—quite a bit below the median privately negotiated rate of $127.81, according to a recent New England Journal of Medicine AI study. Each company has a slightly different business model, but they generally charge providers subscription or licensing fees for their software.
The companies declined to share what they charge for their software. The cameras can cost up to $20,000 and are either purchased separately or wrapped into the software subscription as a rental.
The greater compliance with screening recommendations that the machines make possible, along with a corresponding increase in referrals to specialists, makes it worthwhile, said Lindsie Buchholz, clinical informatics lead at Nebraska Medicine, which in mid-December began using Eyenuk’s system.
“It kind of helps the camera pay for itself,” she said.
Today, Digital Diagnostics’ system is in roughly 600 sites nationwide, according to the company. AEYE Health said its eye exam is used by “low hundreds” of U.S. providers. Eyenuk declined to share specifics about its reach.
The technology continues to advance, with clinical studies for additional cameras—including a handheld imager that can screen patients in the field—and looking at other eye diseases, like glaucoma. The innovations put ophthalmology alongside radiology, cardiology, and dermatology as specialties in which AI innovation is happening fast.
“They are going to come out in the near future—cameras that you can use in street medicine—and it’s going to help a lot of people,” said Espinoza.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Illustration: Mary Delaware
Source images: Dr_Microbe / iStock, berya113 / iStock