Opinion
Imagine if women’s health had the resources it deserves
When I was a pediatrician in Pakistan, I worked for many years in a community on the outskirts of Karachi called Rehri Goth. It was a poor village best known for fishing. But I knew it as a place where pregnant women were anemic, which meant they were more likely to experience postpartum hemorrhage (PPH), the leading cause of maternal death worldwide. Hard-working families in Rehri Goth did their best to earn a living from the Arabian Sea, even as they had to watch one in 10 of their children die before their fifth birthday.
Rehri Goth is not an outlier. During my more than 30 years as a doctor, I have seen time and again how women’s health is overlooked. Women lack access to basic care, and they consistently eat least and last. These biases can create intergenerational ill health. That’s one of the reasons I jumped at the chance to lead the Bill & Melinda Gates Foundation’s gender equality work. I’m consistently frustrated at how little basic knowledge we possess about what to do to improve women’s health. Part of my work at the Gates Foundation is dedicated to filling these gaps.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
The history of women’s health is one of neglect. For too long medical research has revolved around male physiology, despite clear sex and gender differences in health and disease. As a result, much of what is understood as fact about how to treat women’s health lacks a basis in science. For instance, the amount of blood loss needed to “qualify” as PPH was arbitrarily chosen decades ago. The ways in which conditions like asthma or cardiovascular diseases might manifest in women are often misunderstood, which can lead to misdiagnoses and delayed care. Research for conditions that specifically affect women, like endometriosis and menopause, receives a tiny fraction of funding compared to male-specific conditions like erectile dysfunction.
Systemic negligence—including the lack of effective treatments, poor care delivery, and the overall dearth of scientific research that centers women’s health—has driven gender disparities in health outcomes. A January report from the World Economic Forum and McKinsey Health Institute revealed that women spend 25 percent more of their lives in poor health compared to men. This is not because women live longer than men, on average; it’s largely a result of the systematic lack of sex- and gender-specific disease understanding. Billions of women and girls are thus denied the opportunity to be full and active participants at home and in society. Closing the health gap would infuse the global economy with an additional $1 trillion every year, as more women are able to join the workforce, according to the McKinsey report.
Everyone has a right to health care that is evidence-based and appropriate for our bodies. This is not a question of getting marginally better outcomes around the edges. It lies at the very core of gender equality and the well-being of communities around the world depends on it.
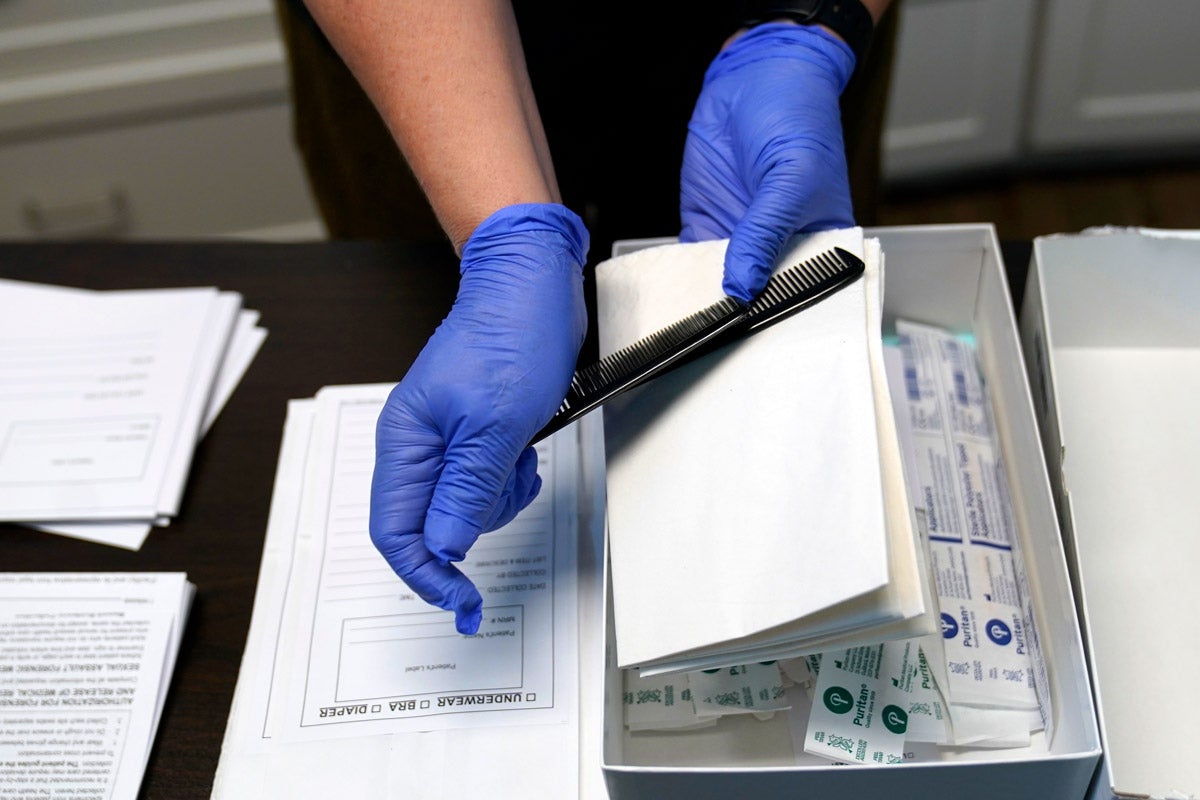
The good news is solutions are closer at hand than we may realize. PPH is the leading cause of maternal death worldwide in part because in the past 30 years, only two new medicines have been developed to manage such severe bleeding. In 2019, the Gates Foundation funded a large international clinical trial, called E-Motive, to determine what bundle of interventions would most effectively prevent maternal death from PPH in low-resource settings.
One of the most useful was serendipitous. Assessing PPH had previously been done by birth attendants eyeballing the size of the pool of blood on the ground. To standardize measurements, initial tests of treatments used a drape to funnel the blood into a container marked with volumes. This led to a clinical trial using a calibrated drape. The trial results, published last year, show the drape helped birth attendants keep better track of blood loss during deliveries, prompting quicker treatment for PPH. The tool was combined with other simple, readily available interventions, such as uterine massage and oxytocin, which together decreased cases of death due to severe bleeding by 60 percent.
Imagine what will happen when there are finally adequate resources devoted to addressing these challenges.
We need more such research and development efforts, and I think we’re going to see them. I am optimistic that funders, policymakers, and researchers are finally seeing both the need and the opportunity to revolutionize women’s health. Recently, building on the launch of First Lady Jill Biden’s White House Initiative on Women’s Health Research, President Joe Biden signed an executive order that expands and prioritizes women’s health across U.S. federal research agencies—including with new funding. The U.K.’s Foreign, Commonwealth and Development Office committed new funding aimed to improve the health of women around the world.
Much of what is understood as fact about how to treat women’s health lacks a basis in science.
In January, I became cochair of a World Economic Forum initiative, the Global Alliance for Women’s Health. This group brings 42 companies, NGOs, and foundations together to bring new resources and attention to women’s health. We’ve garnered more than $50 million in committed new funding to address women’s health by, for example, bridging gaps in menstrual health; increasing access to tools that reduce PPH; encouraging health innovations that meet women’s diverse needs, preferences and lifestyles; and exploring new financing models to increase funding for women’s health.
The Gates Foundation is hoping to make it easier for stakeholders to act. Last year, we partnered with the National Institutes for Health to develop the Women’s Health Innovation Opportunity Map, highlighting 50 high-return opportunities to advance women’s health research. Some, like promoting gender- and sex-specific health research and investing to equip the next generation of women’s health leaders, are already under way. Another way we’re working to make women’s needs and voices central to research and development is by supporting organizations like WomenLift Health, which recently hosted more than 800 people at an international conference in Tanzania focused on advancing women leaders in global health.
These signs of progress demonstrate that decisionmakers are finally starting to pay attention. Thinking about women’s needs, asking how new products and services will affect women, and testing novel medicines in women’s bodies will lead to a burst of progress. I saw this firsthand back in Rehri Goth: We developed a program tailored to the women and children there, and in four years maternal mortality dropped by 70 percent.
Change is possible. We must continue to push. The future health of millions of women and girls depend on it.
Top image source: miakievy / iStock

Republish this article
<p>It’s time for women to be a priority.</p>
<p>Written by Anita Zaidi</p>
<p>This <a rel="canonical" href="https://harvardpublichealth.org/reproductive-health/to-reduce-womens-health-problems-start-by-erasing-inequities/">article</a> originally appeared in<a href="https://harvardpublichealth.org/">Harvard Public Health magazine</a>. Subscribe to their <a href="https://harvardpublichealth.org/subscribe/">newsletter</a>.</p>
<p class="has-drop-cap">When I was a pediatrician in Pakistan, I worked for many years in a community on the outskirts of Karachi called Rehri Goth. It was a poor village best known for fishing. But I knew it as a place where pregnant women were anemic, which meant they were more likely to experience postpartum hemorrhage (PPH), the leading cause of maternal death worldwide. Hard-working families in Rehri Goth did their best to earn a living from the Arabian Sea, even as they had to watch one in 10 of their children die before their fifth birthday.</p>
<p>Rehri Goth is not an outlier. During my more than 30 years as a doctor, I have seen time and again how <a href="https://harvardpublichealth.org/equity/a-qa-with-jen-gunter-the-internets-ob-gyn/" target="_blank" rel="noreferrer noopener">women’s health</a> is overlooked. Women lack access to basic care, and they consistently eat least and last. These biases can create intergenerational ill health. That’s one of the reasons I jumped at the chance to lead the Bill & Melinda Gates Foundation’s gender equality work. I’m consistently frustrated at how little basic knowledge we possess about what to do to improve women’s health. Part of my work at the Gates Foundation is dedicated to filling these gaps.</p>
<p>The history of women’s health is one of neglect. For too long medical research has revolved around male physiology, despite clear sex and gender differences in health and disease. As a result, much of what is understood as fact about how to treat women’s health lacks a basis in science. For instance, the amount of blood loss needed to “qualify” as PPH was arbitrarily chosen decades ago. The ways in which conditions like asthma or cardiovascular diseases might manifest in women are often misunderstood, which can lead to misdiagnoses and delayed care. Research for conditions that specifically affect women, like endometriosis and menopause, receives a tiny fraction of funding compared to male-specific conditions like erectile dysfunction.</p>
<p>Systemic negligence—including the lack of effective treatments, <a href="https://harvardpublichealth.org/equity/a-qa-with-jen-gunter-the-internets-ob-gyn/">poor care delivery</a>, and the overall dearth of scientific research that centers women’s health—has driven gender disparities in health outcomes. A <a href="https://www.mckinsey.com/mhi/our-insights/closing-the-womens-health-gap-a-1-trillion-dollar-opportunity-to-improve-lives-and-economies#/" target="_blank" rel="noreferrer noopener">January report</a> from the World Economic Forum and McKinsey Health Institute revealed that women spend 25 percent more of their lives in poor health compared to men. This is not because women live longer than men, on average; it’s largely a result of the systematic lack of sex- and gender-specific disease understanding. Billions of women and girls are thus denied the opportunity to be full and active participants at home and in society. Closing the health gap would infuse the global economy with an additional $1 trillion every year, as more women are able to join the workforce, according to the McKinsey report.</p>
<p>Everyone has a right to health care that is evidence-based and appropriate for our bodies. This is not a question of getting marginally better outcomes around the edges. It lies at the very core of gender equality and the well-being of communities around the world depends on it.</p>
<p>The good news is solutions are closer at hand than we may realize. PPH is the leading cause of <a href="https://harvardpublichealth.org/policy-practice/maternal-mortality-is-soaring-home-visits-might-help/" target="_blank" rel="noreferrer noopener">maternal death</a> worldwide in part because in the past 30 years, only two new medicines have been developed to manage such severe bleeding. In 2019, the Gates Foundation funded a large international clinical trial, called E-Motive, to determine what bundle of interventions would most effectively prevent maternal death from PPH in low-resource settings.</p>
<p>One of the most useful was serendipitous. Assessing PPH had previously been done by birth attendants eyeballing the size of the pool of blood on the ground. To standardize measurements, initial tests of treatments used a drape to funnel the blood into a container marked with volumes. This led to a clinical trial using a calibrated drape. The trial results, published last year, show the drape helped birth attendants keep better track of blood loss during deliveries, prompting quicker treatment for PPH. The tool was combined with other simple, readily available interventions, such as uterine massage and oxytocin, which together decreased cases of death due to severe bleeding by 60 percent.</p>
<p>Imagine what will happen when there are finally adequate resources devoted to addressing these challenges. </p>
<p>We need more such research and development efforts, and I think we’re going to see them. I am optimistic that funders, policymakers, and researchers are finally seeing both the need and the opportunity to revolutionize women’s health. Recently, building on the launch of First Lady Jill Biden’s White House Initiative on Women’s Health Research, President Joe Biden signed an executive order that expands and prioritizes women’s health across U.S. federal research agencies—including with new funding. The U.K.'s Foreign, Commonwealth and Development Office committed new funding aimed to improve the health of women around the world.</p>
<figure class="wp-block-pullquote alignwide"><blockquote><p>Much of what is understood as fact about how to treat women’s health lacks a basis in science.</p></blockquote></figure>
<p>In January, I became cochair of a World Economic Forum initiative, the Global Alliance for Women’s Health. This group brings 42 companies, NGOs, and foundations together to bring new resources and attention to women’s health. We’ve garnered more than $50 million in committed new funding to address women’s health by, for example, bridging gaps in menstrual health; increasing access to tools that reduce PPH; encouraging health innovations that meet women’s diverse needs, preferences and lifestyles; and exploring new financing models to increase funding for women’s health.</p>
<p>The Gates Foundation is hoping to make it easier for stakeholders to act. Last year, we partnered with the National Institutes for Health to develop the <a href="https://orwh.od.nih.gov/sites/orwh/files/docs/womens-health-rnd-opportunity-map_2023_508.pdf" target="_blank" rel="noreferrer noopener">Women’s Health Innovation Opportunity Map</a>, highlighting 50 high-return opportunities to advance women’s health research. Some, like promoting gender- and sex-specific health research and investing to equip the next generation of women’s health leaders, are already under way. Another way we’re working to make women's needs and voices central to research and development is by supporting organizations like WomenLift Health, which recently hosted more than 800 people at an international conference in Tanzania focused on advancing women leaders in global health.</p>
<p>These signs of progress demonstrate that decisionmakers are finally starting to pay attention. Thinking about women’s needs, asking how new products and services will affect women, and testing novel medicines in women’s bodies will lead to a burst of progress. I saw this firsthand back in Rehri Goth: We developed a program tailored to the women and children there, and in four years maternal mortality dropped by 70 percent.</p>
<p class=" t-has-endmark t-has-endmark">Change is possible. We must continue to push. The future health of millions of women and girls depend on it.</p>
<script async src="https://www.googletagmanager.com/gtag/js?id=G-S1L5BS4DJN"></script>
<script>
window.dataLayer = window.dataLayer || [];
if (typeof gtag !== "function") {function gtag(){dataLayer.push(arguments);}}
gtag('js', new Date());
gtag('config', 'G-S1L5BS4DJN');
</script>
Republishing guidelines
We’re happy to know you’re interested in republishing one of our stories. Please follow the guidelines below, adapted from other sites, primarily ProPublica’s Steal Our Stories guidelines (we didn’t steal all of its republishing guidelines, but we stole a lot of them). We also borrowed from Undark and KFF Health News.
Timeframe: Most stories and opinion pieces on our site can be republished within 90 days of posting. An article is available for republishing if our “Republish” button appears next to the story. We follow the Creative Commons noncommercial no-derivatives license.
When republishing a Harvard Public Health story, please follow these rules and use the required acknowledgments:
- Do not edit our stories, except to reflect changes in time (for instance, “last week” may replace “yesterday”), make style updates (we use serial commas; you may choose not to), and location (we spell out state names; you may choose not to).
- Include the author’s byline.
- Include text at the top of the story that says, “This article was originally published by Harvard Public Health. You must link the words “Harvard Public Health” to the story’s original/canonical URL.
- You must preserve the links in our stories, including our newsletter sign-up language and link.
- You must use our analytics tag: a single pixel and a snippet of HTML code that allows us to monitor our story’s traffic on your site. If you utilize our “Republish” link, the code will be automatically appended at the end of the article. It occupies minimal space and will be enclosed within a standard <script> tag.
- You must set the canonical link to the original Harvard Public Health URL or otherwise ensure that canonical tags are properly implemented to indicate that HPH is the original source of the content. For more information about canonical metadata, click here.
Packaging: Feel free to use our headline and deck or to craft your own headlines, subheads, and other material.
Art: You may republish editorial cartoons and photographs on stories with the “Republish” button. For illustrations or articles without the “Republish” button, please reach out to republishing@hsph.harvard.edu.
Exceptions: Stories that do not include a Republish button are either exclusive to us or governed by another collaborative agreement. Please reach out directly to the author, photographer, illustrator, or other named contributor for permission to reprint work that does not include our Republish button. Please do the same for stories published more than 90 days previously. If you have any questions, contact us at republishing@hsph.harvard.edu.
Translations: If you would like to translate our story into another language, please contact us first at republishing@hsph.harvard.edu.
Ads: It’s okay to put our stories on pages with ads, but not ads specifically sold against our stories. You can’t state or imply that donations to your organization support Harvard Public Health.
Responsibilities and restrictions: You have no rights to sell, license, syndicate, or otherwise represent yourself as the authorized owner of our material to any third parties. This means that you cannot actively publish or submit our work for syndication to third-party platforms or apps like Apple News or Google News. Harvard Public Health recognizes that publishers cannot fully control when certain third parties aggregate or crawl content from publishers’ own sites.
You may not republish our material wholesale or automatically; you need to select stories to be republished individually.
You may not use our work to populate a website designed to improve rankings on search engines or solely to gain revenue from network-based advertisements.
Any website on which our stories appear must include a prominent and effective way to contact the editorial team at the publication.
Social media: If your publication shares republished stories on social media, we welcome a tag. We are @PublicHealthMag on X, Threads, and Instagram, and Harvard Public Health magazine on Facebook and LinkedIn.
Questions: If you have other questions, email us at republishing@hsph.harvard.edu.