People
Bringing public health data into the 21st century
Public health data in the U.S. suffers from underfunded, antiquated systems built around siloed, single-purpose databases, spreadsheets, and even faxes. Fixing these problems is the job of Jennifer Layden, who is an epidemiologist, a physician, and the director of the Office of Public Health Data, Surveillance, and Technology at the Centers for Disease Control and Prevention. She leads the CDC’s Data Modernization Initiative, established in 2019.
Layden knows well the challenges of data management across the system. Before she worked at the CDC, she spent nearly four years as state epidemiologist and chief medical officer at the Illinois Department of Public Health. Her time in Chicago introduced her to the data challenges at what the CDC calls the “State, Tribal, Local, and Territorial (STLT), or “jurisdictional” level. At the outset of the COVID-19 pandemic, she was the deputy commissioner and chief medical officer for the Chicago Department of Public Health. In September 2020, she joined the CDC’s Office of Science to help lead the agency’s COVID response.
Occupying much of her attention is an ambitious plan known as HTI-2, shorthand for Health Data, Technology, and Interoperability: Patient Engagement, Information Sharing, and Public Health Interoperability. (Its predecessor, HTI-1, addressed health data interoperability generally but did not include a focus on public health.) Her office has adopted a public health data strategy, a two-year roadmap of the administrative actions needed on data, technology, policy and administrative actions to meet public health data goals.
Layden talked with Harvard Public Health contributor Elizabeth Gardner about the challenges of modernizing public health data.
This conversation has been edited for length and clarity.
Harvard Public Health: Have you always been a health data geek?

Jennifer Layden: I’ve always loved modeling and epidemiological studies, which were the basis of my Ph.D. work. I became passionate about data modernization when I started working at the jurisdiction level [and] realized how antiquated the systems were and how much they limited what we could do. I wanted to really understand the barriers, so I started to work on modernization efforts, particularly in Chicago, where we collaborated with academic and private partners to improve data exchange.
Then I jumped right into that area at the CDC because I recognized the need, not just at the CDC, but in the whole broad ecosystem of data exchange nationally. We need to address a boom-and-bust pattern in public health data where some crisis happens and a significant amount of money is directed to public health, and then the crisis goes away [and] modernizing and improving our systems is no longer top of mind, and the funding also goes away.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
HPH: What was your most successful project from your time at the state and local level?
Layden: The reporting system we set up in Chicago at the start of COVID-19. Providers had to report cases to public health. The system just couldn’t keep up [with the volume of cases], and many facilities were still sending us data by fax or Excel file.
We wrote a public health order, defining the minimum essential data to submit for public health purposes for COVID—and the standard formats for that data—and requiring it to be submitted electronically. We partnered with a hospital [Rush University Medical Center] that stood up a cloud-based hub for us to receive that data. Within a short time, we were able to receive electronic submissions of these data elements for the confirmed COVID cases.
HPH: Much of public health data is locked up in disease-specific siloes. Is there a path to breaking those siloes down?
Layden: That pattern is largely because of a disease-specific approach to funding, which has led to each program or disease area developing their own way of doing things.
So if you take, for example, measles—our measles program has certain data elements that they request from jurisdictions. But at the same time, there’s a notifiable disease program that also needs measles data. So you now have two systems. It’s more than two, actually, and I don’t want to pick on measles at all. A colleague in Tennessee analyzed reporting requirements for 11 “notifiable” diseases and found that jurisdictions had to report data to multiple systems for all of them.
So one of the things that we’re very committed to, and it’s not going to happen overnight, is streamlining all that, integrating our processes for requesting the data and leveraging data and technology standards. There’s a clear path to get there, but it does require addressing not just the technical but the policy and processing barriers.
HPH: There are a lot of people involved in these efforts. How do they get a feeling of being at the table?
Layden: Our teams work hand in hand with jurisdictions. We don’t just say, “This is the solution.” We take a human-centered design approach. What are their needs? What are their end uses for the data? What challenges are they facing to get there?
We hear that the manual entry of data is too taxing. We hear uncertainty about how the data is being used. People want to know what these changes mean for their workforce: Do they need to train staff? Do they need new types of expertise? And is funding sustainable? They don’t want to give up systems, like their Excel files, that might be antiquated and slow before knowing that these new systems not only work but are sustainable.
We held a summit [in August] to take what we’ve heard, identify the recurrent themes, and figure out how to make the changes that we need. We want to build out a broader data governance process that enables active participation from STLTs in a way that’s nimble and flexible.
HPH: If you could wave your hand and get rid of one obstacle to the free flow of complete, accurate public health data, which one would you start with and why?
Layden: Funding. It doesn’t solve everything—you still have to address policy, governance, culture, change management, and all that—but if people don’t know they have sufficient funding, they will be skeptical about whether they can make the transition.
We gave the health IT side of the house $35 billion to modernize, right? We’re just at the infancy stage with public health, with a few billion over four to five years. Maybe it’s not the level of funding that everyone would want, but at least knowing there’s a sustained path will ease a lot of concerns and enable acceleration of priority work.
HPH: How nimble is the public health system to deal with novel disease threats? And how is that going to get better with the changes you’re making?
Layden: We are better off than we were a few years ago. We can quickly adapt electronic case reporting to be applicable to another condition. But there are still some gaps on the policy side around data-sharing agreements.
Because there’s not a federal authority to require data to be sent to CDC every time there’s a new condition, it’s a round of negotiations with each jurisdiction. We’re building up data governance capabilities to streamline that process. We haven’t made significant progress on establishing that kind of authority yet, but we’re continuing on that path while we work on data usage agreements and reporting standards around HTI-2.
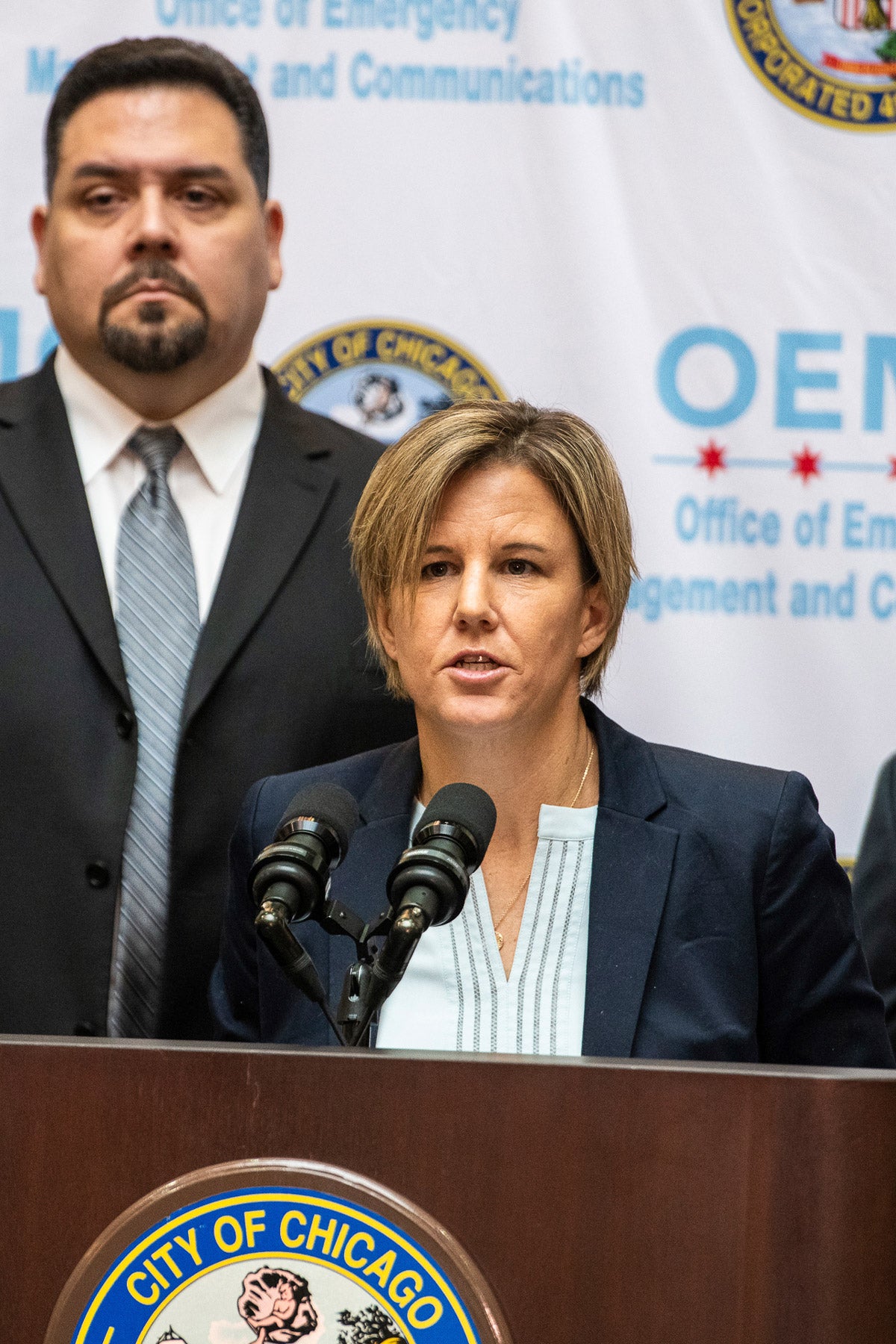
Top image: Jennifer Layden speaks at a news conference in Chicago in January 2020, when she was the chief medical officer of the Illinois Department of Public Health. (Tyler LaRiviere / Chicago Sun-Times via AP Photos)
Republish this article
<p>In the U.S., data is handled differently for every disease. Jennifer Layden hopes to improve that system.</p>
<p>Written by Elizabeth Gardner</p>
<p>This <a rel="canonical" href="https://harvardpublichealth.org/policy-practice/public-health-data-management-needs-fixing-heres-how-we-do-it/">article</a> originally appeared in<a href="https://harvardpublichealth.org/">Harvard Public Health magazine</a>. Subscribe to their <a href="https://harvardpublichealth.org/subscribe/">newsletter</a>.</p>
<p class="has-drop-cap">Public health data in the U.S. suffers from underfunded, antiquated systems built around siloed, single-purpose databases, spreadsheets, and even faxes. Fixing these problems is the job of Jennifer Layden, who is an epidemiologist, a physician, and the director of the Office of Public Health Data, Surveillance, and Technology at the Centers for Disease Control and Prevention. She leads the CDC’s Data Modernization Initiative, established in 2019.</p>
<p>Layden knows well the challenges of data management across the system. Before she worked at the CDC, she spent nearly four years as state epidemiologist and chief medical officer at the Illinois Department of Public Health. Her time in Chicago introduced her to the data challenges at what the CDC calls the “State, Tribal, Local, and Territorial (STLT), or “jurisdictional” level. At the outset of the COVID-19 pandemic, she was the deputy commissioner and chief medical officer for the Chicago Department of Public Health. In September 2020, she joined the CDC’s Office of Science to help lead the agency’s COVID response.</p>
<p>Occupying much of her attention is an ambitious plan known as HTI-2, shorthand for Health Data, Technology, and Interoperability: Patient Engagement, Information Sharing, and Public Health Interoperability. (Its predecessor, <a href="https://www.healthit.gov/topic/laws-regulation-and-policy/health-data-technology-and-interoperability-certification-program" target="_blank" rel="noreferrer noopener">HTI-1</a>, addressed health data interoperability generally but did not include a focus on public health.) Her office has adopted a <a href="https://www.cdc.gov/ophdst/public-health-data-strategy/index.html" target="_blank" rel="noreferrer noopener">public health data strategy</a>, a two-year roadmap of the administrative actions needed on data, technology, policy and administrative actions to meet public health data goals.</p>
<p>Layden talked with <em>Harvard Public Health</em> contributor Elizabeth Gardner about the challenges of modernizing public health data.</p>
<p><em>This conversation has been edited for length and clarity.</em></p>
<p><strong><em>Harvard Public Health</em>: </strong>Have you always been a health data geek?</p>
<p><strong>Jennifer Layden: </strong>I’ve always loved modeling and epidemiological studies, which were the basis of my Ph.D. work. I became passionate about data modernization when I started working at the jurisdiction level [and] realized how antiquated the systems were and how much they limited what we could do. I wanted to really understand the barriers, so I started to work on modernization efforts, particularly in Chicago, where we collaborated with academic and private partners to improve data exchange.</p>
<p>Then I jumped right into that area at the CDC because I recognized the need, not just at the CDC, but in the whole broad ecosystem of data exchange nationally. We need to address a boom-and-bust pattern in public health data where some crisis happens and a significant amount of money is directed to public health, and then the crisis goes away [and] modernizing and improving our systems is no longer top of mind, and the funding also goes away.</p>
<p><strong>HPH: </strong>What was your most successful project from your time at the state and local level?</p>
<p><strong>Layden: </strong>The reporting system we set up in Chicago at the start of COVID-19. Providers had to report cases to public health. The system just couldn’t keep up [with the volume of cases], and many facilities were still sending us data by fax or Excel file.</p>
<p>We wrote a public health order, defining the minimum essential data to submit for public health purposes for COVID—and the standard formats for that data—and requiring it to be submitted electronically. We partnered with a hospital [Rush University Medical Center] that stood up a <a href="https://pubmed.ncbi.nlm.nih.gov/35544440/" target="_blank" rel="noreferrer noopener">cloud-based hub</a> for us to receive that data. Within a short time, we were able to receive electronic submissions of these data elements for the confirmed COVID cases.</p>
<p><strong>HPH: </strong>Much of public health data is locked up in disease-specific siloes. Is there a path to breaking those siloes down?</p>
<p><strong>Layden: </strong>That pattern is largely because of a disease-specific approach to funding, which has led to each program or disease area developing their own way of doing things.</p>
<p>So if you take, for example, measles—our measles program has certain data elements that they request from jurisdictions. But at the same time, there’s a notifiable disease program that also needs measles data. So you now have two systems. It's more than two, actually, and I don't want to pick on measles at all. A colleague in Tennessee <a href="https://healthdata.tn.gov/Health-Data-Tools/Analysis-of-National-Notifiable-Disease-Reporting-/apbk-k5nz/about_data" target="_blank" rel="noreferrer noopener">analyzed reporting requirements for 11 “notifiable” diseases</a> and found that jurisdictions had to report data to multiple systems for all of them.</p>
<p>So one of the things that we're very committed to, and it's not going to happen overnight, is streamlining all that, integrating our processes for requesting the data and leveraging data and technology standards. There's a clear path to get there, but it does require addressing not just the technical but the policy and processing barriers.</p>
<p><strong>HPH: </strong>There are a lot of people involved in these efforts. How do they get a feeling of being at the table?</p>
<p><strong>Layden: </strong>Our teams work hand in hand with jurisdictions. We don’t just say, “This is the solution.” We take a human-centered design approach. What are their needs? What are their end uses for the data? What challenges are they facing to get there?</p>
<p>We hear that the manual entry of data is too taxing. We hear uncertainty about how the data is being used. People want to know what these changes mean for their workforce: Do they need to train staff? Do they need new types of expertise? And is funding sustainable? They don’t want to give up systems, like their Excel files, that might be antiquated and slow before knowing that these new systems not only work but are sustainable.</p>
<p>We held a summit [in August] to take what we’ve heard, identify the recurrent themes, and figure out how to make the changes that we need. We want to build out a broader data governance process that enables active participation from STLTs in a way that’s nimble and flexible.</p>
<p><strong>HPH:</strong> If you could wave your hand and get rid of one obstacle to the free flow of complete, accurate public health data, which one would you start with and why?</p>
<p><strong>Layden: </strong>Funding. It doesn’t solve everything—you still have to address policy, governance, culture, change management, and all that—but if people don’t know they have sufficient funding, they will be skeptical about whether they can make the transition.</p>
<p>We <a href="https://crsreports.congress.gov/product/pdf/R/R40161" target="_blank" rel="noreferrer noopener">gave the health IT</a> side of the house $35 billion to modernize, right? We’re just at the infancy stage with public health, with a few billion over four to five years. Maybe it’s not the level of funding that everyone would want, but at least knowing there’s a sustained path will ease a lot of concerns and enable acceleration of priority work.</p>
<p><strong>HPH: </strong>How nimble is the public health system to deal with novel disease threats? And how is that going to get better with the changes you’re making?</p>
<p><strong>Layden: </strong>We are better off than we were a few years ago. We can quickly adapt electronic case reporting to be applicable to another condition. But there are still some gaps on the policy side around data-sharing agreements.</p>
<p class=" t-has-endmark t-has-endmark">Because there's not a federal authority to require data to be sent to CDC every time there's a new condition, it's a round of negotiations with each jurisdiction. We’re building up data governance capabilities to streamline that process. We haven’t made significant progress on establishing that kind of authority yet, but we’re continuing on that path while we work on data usage agreements and reporting standards around HTI-2.</p>
<script async src="https://www.googletagmanager.com/gtag/js?id=G-S1L5BS4DJN"></script>
<script>
window.dataLayer = window.dataLayer || [];
if (typeof gtag !== "function") {function gtag(){dataLayer.push(arguments);}}
gtag('js', new Date());
gtag('config', 'G-S1L5BS4DJN');
</script>
Republishing guidelines
We’re happy to know you’re interested in republishing one of our stories. Please follow the guidelines below, adapted from other sites, primarily ProPublica’s Steal Our Stories guidelines (we didn’t steal all of its republishing guidelines, but we stole a lot of them). We also borrowed from Undark and KFF Health News.
Timeframe: Most stories and opinion pieces on our site can be republished within 90 days of posting. An article is available for republishing if our “Republish” button appears next to the story. We follow the Creative Commons noncommercial no-derivatives license.
When republishing a Harvard Public Health story, please follow these rules and use the required acknowledgments:
- Do not edit our stories, except to reflect changes in time (for instance, “last week” may replace “yesterday”), make style updates (we use serial commas; you may choose not to), and location (we spell out state names; you may choose not to).
- Include the author’s byline.
- Include text at the top of the story that says, “This article was originally published by Harvard Public Health. You must link the words “Harvard Public Health” to the story’s original/canonical URL.
- You must preserve the links in our stories, including our newsletter sign-up language and link.
- You must use our analytics tag: a single pixel and a snippet of HTML code that allows us to monitor our story’s traffic on your site. If you utilize our “Republish” link, the code will be automatically appended at the end of the article. It occupies minimal space and will be enclosed within a standard <script> tag.
- You must set the canonical link to the original Harvard Public Health URL or otherwise ensure that canonical tags are properly implemented to indicate that HPH is the original source of the content. For more information about canonical metadata, click here.
Packaging: Feel free to use our headline and deck or to craft your own headlines, subheads, and other material.
Art: You may republish editorial cartoons and photographs on stories with the “Republish” button. For illustrations or articles without the “Republish” button, please reach out to republishing@hsph.harvard.edu.
Exceptions: Stories that do not include a Republish button are either exclusive to us or governed by another collaborative agreement. Please reach out directly to the author, photographer, illustrator, or other named contributor for permission to reprint work that does not include our Republish button. Please do the same for stories published more than 90 days previously. If you have any questions, contact us at republishing@hsph.harvard.edu.
Translations: If you would like to translate our story into another language, please contact us first at republishing@hsph.harvard.edu.
Ads: It’s okay to put our stories on pages with ads, but not ads specifically sold against our stories. You can’t state or imply that donations to your organization support Harvard Public Health.
Responsibilities and restrictions: You have no rights to sell, license, syndicate, or otherwise represent yourself as the authorized owner of our material to any third parties. This means that you cannot actively publish or submit our work for syndication to third-party platforms or apps like Apple News or Google News. Harvard Public Health recognizes that publishers cannot fully control when certain third parties aggregate or crawl content from publishers’ own sites.
You may not republish our material wholesale or automatically; you need to select stories to be republished individually.
You may not use our work to populate a website designed to improve rankings on search engines or solely to gain revenue from network-based advertisements.
Any website on which our stories appear must include a prominent and effective way to contact the editorial team at the publication.
Social media: If your publication shares republished stories on social media, we welcome a tag. We are @PublicHealthMag on X, Threads, and Instagram, and Harvard Public Health magazine on Facebook and LinkedIn.
Questions: If you have other questions, email us at republishing@hsph.harvard.edu.


