Feature
A National Weather Service for disease?
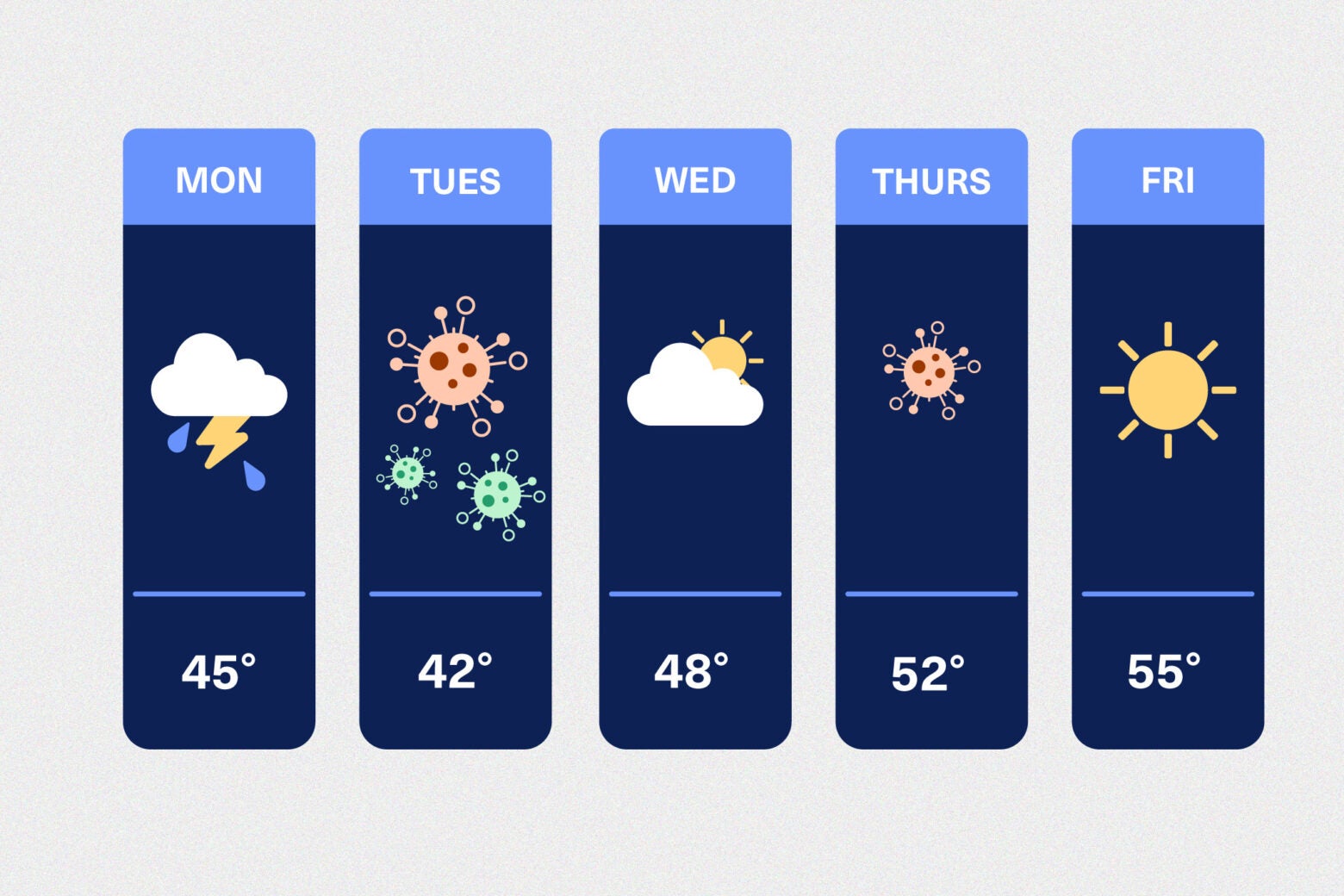
Can we predict the ebb and flow of infectious disease the way meteorologists predict the weather?
The federal government has bet big on the concept with a new nationwide network called Insight Net, which links academic disease modelers with public health practitioners. The network comprises 13 research consortia with participants in 24 states and is funded with up to $262 million from the Centers for Disease Control and Prevention (CDC). Insight Net members are piloting analytical techniques that combine novel data sources to guide surveillance and inform decision-making during outbreaks. The end goal is to create something akin to a National Weather Service for disease.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
Such capacity would be a game-changer for state and local health authorities and for hospitals. At the height of the COVID-19 pandemic, “we were not good at forecasting the demand,” says Douglas Sawyer, chief academic officer of MaineHealth, that state’s biggest hospital system. “We didn’t steer the ship, so to speak, with high fidelity as we wish we could have. We couldn’t prepare and shift resources in thoughtful ways.”
Many hospitals struggled with the crush of patients who needed intensive, isolated care. Because hospitals could not accurately predict the size of impending infection waves, many delayed or canceled routine health care such as physicals or cancer screenings. Meanwhile, Covid care sites built or converted by federal and state authorities ended up being largely unneeded.
These forecasting issues had serious financial consequences for hospitals—and serious health consequences for the public. Insight Net’s progress toward closing that information gap has been steady and marked by small but important victories—as well as plenty of reminders that even the best forecasts are only as good as the data that feed them.
Forecasting more than the next crisis
By linking people working in public health directly with disease modelers, the CDC aims to fix the ad hoc approach it used for pandemic forecasting, which was panned from almost the start. In the summer of 2020, a critique in Foreign Affairs labeled the CDC’s approach “an arbitrary assortment of academics” reacting on the fly and asserted no one today would handle hurricane response in that fashion. In 2021, the CDC tapped Caitlin Rivers, one of the article’s coauthors and an epidemiologist at Johns Hopkins Bloomberg School of Public Health, as the first associate director of its new Center for Forecasting and Outbreak Analytics (CFA). In 2023 the CFA established Insight Net, and Rivers, who had returned to Johns Hopkins, became director of its node in the network (Dylan George, her Foreign Affairs coauthor, is the CFA’s current director). Their core message, then and now: Disease forecasting shouldn’t be improvised.
Policymakers and the public put their trust in major storm alerts, according to George, because the weather service is “applying the best models in an operational context on a day in and day out basis, cranking out results,” George says. “And then you have local meteorologists interpret those results for people to actually make decisions.” That process establishes a track record of monitoring and communicating forecasts, including their uncertainty, even when the weather is calm, sunny, and mild. “We’ve tried to pattern after that,” George adds.
That has meant investing in a dedicated program for disease forecasting, with formal working relationships between modelers and federal, state, and local health officials. It also means the CFA has been keen to demonstrate how modeling can help public health practice and communication. For instance, it has tapped data from the National Wastewater Surveillance System, launched by the CDC in 2020, to improve localized forecasts of Covid hospital admissions. It also helped the Chicago Department of Public Health confront a March 2024 measles outbreak at a temporary migrant shelter housing more than 1,400 people. As public health workers began vaccinating and screening shelter residents to identify and isolate the sick, department leaders reached out to the CFA, which rapidly refined a model of measles to mimic the outbreak’s timeline of infection, symptom onset, and recovery, which Chicago health officials could then use to predict its future course.
The model didn’t influence the department’s interventions, which were already underway. But it did reassure officials they’d correctly identified their patient zero: Outbreak simulations that assumed earlier, undetected infections generated far different case data from what was observed. The forecasts also helped set expectations for the outbreak’s severity by providing a range of potential case numbers and dates when infections would peak and subside. After a couple weeks of continuous updating with data on new measles cases, the model predicted there would be between 57 and 65 cases and the final rash would appear on April 16. In the end, the outbreak lasted about two months and infected 57 people.
“It really helped our own planning, and our thinking about staffing,” says Stephanie Gretsch, an epidemiologist at the Chicago Department of Public Health. “It was also incredibly helpful for communicating with our city agency partners responsible for housing and schooling; and the hospitals we asked to help isolate infected residents, to give them a sense of how long we thought this was going to last.”
After the outbreak, Chicago public health officials used the modeling to quantify the value of its interventions. Outbreak simulations where responses did not include mass vaccination or active case-finding efforts suggested it would have lasted seven weeks longer and more than quadrupled the number of infections. This finding suggests that modeling hypothetical scenarios might offer a tool for easing heightened skepticism of public health interventions and investments, say several Insight Net partners.
Insight Net forecasters are … mixing traditional data sources such as infection rates with the digital breadcrumbs of human activity like searches for symptoms, social media posts, and trends in medication purchases.
Syphilis is one target of the Insight Net consortium at the University of Utah. The disease, resurgent in the U.S., can infect a fetus during pregnancy and cause serious medical complications, including miscarriage, stillbirth, and infant death. The goal is to “address the issues and show how bad this problem could get if trends continue,” says principal investigator Matthew Samore, a professor of medicine and the division chief of epidemiology at the University of Utah. “We also want to get a deeper understanding of how STIs like this are spreading through different populations…and to calculate how much benefit do we get by investing in more intensive screening and contact tracing.” By helping establish the extent of the risk, the models could bolster requests to fund more screening and treatment of groups with high infection rates, such as people in prison.
The modeling could also improve disease forecasting dashboards used by the public to assess health threats. The Massachusetts Department of Public Health (MDPH) has dashboards that track severe respiratory illnesses statewide, but delays in data reporting from local hospitals limit their usefulness. In 2024, MDPH worked with the Insight Net researchers at the University of Massachusetts Amherst and the University of Texas at Austin to build models filling in those gaps, allowing it to add recent emergency room visits and hospital admissions due to Covid, RSV, and influenza broken down by demographics. Such small-scale adoptions are needed both to validate disease forecasting and to build trust in the models, says Meagan Burns, a senior informatics epidemiologist at MDPH. “These tools are very cool, but they’re also very new,” she says.
People in Massachusetts also are getting a look at disease forecasts as part of their weather news. In February, meteorologists at Boston’s CBS affiliate, WBZ-TV, began adding localized disease data visualizations to their weather reports. These are put together by the Insight Net team based at Johns Hopkins and arranged through a collaboration with the American Meteorological Society. The first one featured a colorful chart showing that emergency room visits due to COVID-19 were declining steadily from their post-Christmas peak. The original plan was to do weekly check-ins on infectious respiratory illnesses, but as the weather warmed, infection numbers plummeted and stayed low.
“There were several weeks where there wasn’t a whole lot to talk about with Covid or the flu,” says meteorologist Terry Eliasen, executive producer of WBZ’s weather team. While viewers might find sunny weather forecasts useful, there didn’t seem to be much news value in “sunny” public health numbers. So WBZ skipped a few weeks. Then Eliasen asked the Johns Hopkins team what else it could do. Over the summer, researchers responded with data visualizations related to outbreaks of norovirus and eastern equine encephalitis, as well as the risk of heat-related illnesses.
This quick shift in focus drew praise as a sign that the university-based modelers at Insight Net are serious about partnering with public health practitioners and communicators. The CFA worked with the Council of State and Territorial Epidemiologists (CTSE) on the legal and logistical issues of data-sharing, and to see what forecasting tools might be useful to its members. The two organizations convened a series of meetings with state and local health officials to ask what uses they might have for forecasting tools and whether there were specialized techniques they’d like. That was especially useful, says Janet Hamilton, the CSTE’s executive director. “We need to have enough time to talk to the modelers to say, ‘That’s a great model but it doesn’t help me. It doesn’t answer my questions.’”
Fixing public health data: everything, everywhere, all at once
Disease threats do not yet have the color-coded, real-time tracking maps the National Weather Service uses for potential hurricanes. Of course, there are no satellite images of developing disease threats, which not only are propelled by unique (and often mutating) biology, but also have to account for something that’s even harder to predict—human behavior. Several Insight Net forecasters are trying to meet this massive data challenge by mixing traditional data sources such as infection rates with the digital breadcrumbs of human activity like searches for symptoms, social media posts, and trends in medication purchases.
People spread diseases when they travel and gather, notes Alessandro “Alex” Vespignani, a physicist and computational scientist at Northeastern University whose lab models large-scale complex systems. He and his team are part of an Insight Net research consortium with Maine’s major hospital systems, MaineHealth and Northern Light Health, which are working on a pilot project to weave human mobility data into disease models. They draw on aggregated and anonymized mobile device location data, databases of global flight schedules, and traces of pathogens found in wastewater sampled from municipal sources and from international flights for analysis by the Boston biotech company Ginkgo Bioworks.
“Our models are like a layer cake,” Vespignani says, with each layer creating a virtual “business as usual world” the modelers use for outbreak simulations. Layers are only added if they significantly improve the model’s predictions or extend the timeline for an accurate forecast. For instance, the lab found that it could accurately forecast greater Boston hospital admission rates three weeks ahead of time by adding mobility and proximity data derived from about 82,000 mobile phones, compared to just two weeks using conventional public health data such as statewide Covid test results. That extra week for planning is “a big deal for hospitals” for scheduling staff and procedures, says Samuel Scarpino, director of Northeastern University’s Institute for Experiential AI and a member of the Insight Net team. Since hospitals aim for 90 percent capacity, even a slight uptick in the need for beds can complicate care.
This fall, the lab will tap retrospective data from Maine’s Covid hospitalization numbers to try to replicate that forecasting capability. It’s also planning to use the mobility-enhanced models to forecast hospitalizations for flu, RSV, and Covid at individual Maine hospitals for the winter of 2024-25. If these efforts are successful, Scarpino hopes to scale the models for use nationwide.
The Insight Net initiative also faces the labyrinthine way the U.S. gathers and shares core public health data such as test results and hospital records. Reducing those obstacles is a key target of the CDC’s Data Modernization Initiative, launched in 2019 to promote things like electronic case reporting, interoperability among different data collection systems, and standardized data use agreements between state, tribal, local and territorial, and federal health authorities. But the data pipeline’s bottlenecks aren’t simply technical and legal, according to infectious disease experts such as Jennifer Nuzzo, an epidemiologist who directs Brown University’s Pandemic Center. They also involve whether we’re asking the right questions about disease threats to get the data we need. “It’s great for us to invest in analytic approaches that can help us tell what could happen in the future,” says Nuzzo. “But what I want to see is a better utilization, analysis, and visualization of the data that we have to tell us what’s happening today.”
If pandemics were hurricanes, having the avian flu virus circulating in cows along with regular flu infections in humans would be akin to a low pressure system in the Caribbean: It could dissipate, but it could also develop into huge trouble for the mainland United States.
For instance, the fragmented efforts to track the H5N1 bird flu virus in the U.S. have drawn a chorus of concern from public health leaders and researchers. Earlier this year, the virus leapt from wild birds to more than 100 million poultry in 49 states as well as other domesticated species, including dairy cows and, more recently, pigs. A small but growing number of people have also been infected (mostly farm workers, but not all). Tracking the virus requires coordination among multiple federal agencies, including the Department of Agriculture, the Food and Drug Administration, and the CDC, as well as states that vary widely in the ways they test animals, people, and bulk milk tanks. The only federally mandated H5N1 screening is for lactating dairy cows being moved across state lines.
Thus far, most humans with bird flu have had minor symptoms, and there’s no evidence of the virus spreading from person to person, which could trigger a pandemic. But the risk increases with flu season, because different viruses infecting the same host can swap genes (known as genetic reassortment) and evolve into something new and more dangerous. If pandemics were hurricanes, having the avian flu virus circulating in cows along with regular flu infections in humans would be akin to a low pressure system in the Caribbean—it could dissipate, but it could also develop into huge trouble for the mainland United States. Nuzzo says we could better predict the outcome if we focused more on targeted surveillance about emerging health threats.
“An awareness of what’s happening this week, and last week, is the starting point for trying to figure out what’s going to happen in the next few weeks and beyond,” says Roni Rosenfeld, a professor of machine learning, language technologies, computer science, and computational biology in the School of Computer Science at Carnegie Mellon University and a cofounder of the Delphi Research Group, a global network of disease modelers working with Insight Net. “So, already before the pandemic, we shifted much of our effort to what I call situational awareness—being aware of what’s happening right now at as fine a geographic, pathogenic, syndromic, and demographic granularity as possible.”
Dylan George, director of the CFA, agrees that disease forecasts will require better raw data and more proactive surveillance. He argues now is the time to strengthen partnerships between researchers and public health practitioners, to build trust and a shared language, and to smooth frictions that can cripple effective collaboration during a crisis. The ultimate test of success for Insight Net, he says, will be seeing them in action:
“If a bunch of state and local health department folks are saying, ‘These forecasting tools are helping me do my job better,’ then I know that we deserve to live another day.”
Illustration: Mary Delaware / Source images: Adobe Stock


