Ideas
As more youth struggle with behavior, clinicians are partnering with lawyers to help
This story was produced by The Hechinger Report, a nonprofit, nonpartisan news outlet focused on education.
Every night before going to bed, Antonio would tuck in his three younger siblings. After school, he’d tinker with toy cars, or help his dad, a mechanic, fix things around the house.
“He’s quiet, but he’s caring in his own way,” said his mother, Yanelie Marquez. The Hechinger Report is using her son’s middle name to protect his privacy.
But four years ago, then-12-year-old Antonio suddenly lost interest in everything and everyone. It started with school: He complained he couldn’t focus or understand the teacher’s instructions. “I’d open up his notebooks, and they were completely empty,” Marquez said.
Then Antonio’s behavior began to change, too: He stopped showering and coming downstairs for dinner. Eventually, he refused to leave his room. And whenever Marquez would ask about his day, he would throw a tantrum.
“He’d say, ‘None of the teachers like me, I hate it,’ and then he’d take that anger out on himself,” she said.
Worried that Antonio was struggling with depression, his mother enrolled him in therapy at Yale Child Study Center in New Haven, Connecticut.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
After ruling out stressors in Antonio’s family environment, the Yale team learned more about the challenges he was facing at school, including severe learning difficulties in the classroom and bullies outside of school. And though the clinicians did everything they could do to help address those behavioral health stressors on their own, they realized they needed another team member to help: a lawyer.
This teamwork comes through Yale Child Study Center’s Medical-Legal Partnership—a collaboration in which health and law professionals team up to address patients’ “health-harming legal needs,” from food and housing to public benefits and school supports. Their unique partnership functions as a kind of legal prescription. To treat a child’s behavioral health symptoms, clinicians and lawyers target the root cause, which can sometimes be a school environment where the child’s legally enshrined academic and emotional needs aren’t being met.
Though the concept of medical-legal partnerships has existed since the 1990s, the Yale partnership, launched in November 2020, is the first in the nation focused exclusively on children’s behavioral health. Last year, the U.S. Department of Health and Human Services invested $1.6 million in the first federally funded demonstration program for medical-legal partnerships, including one at Yale, focused in primary health care.
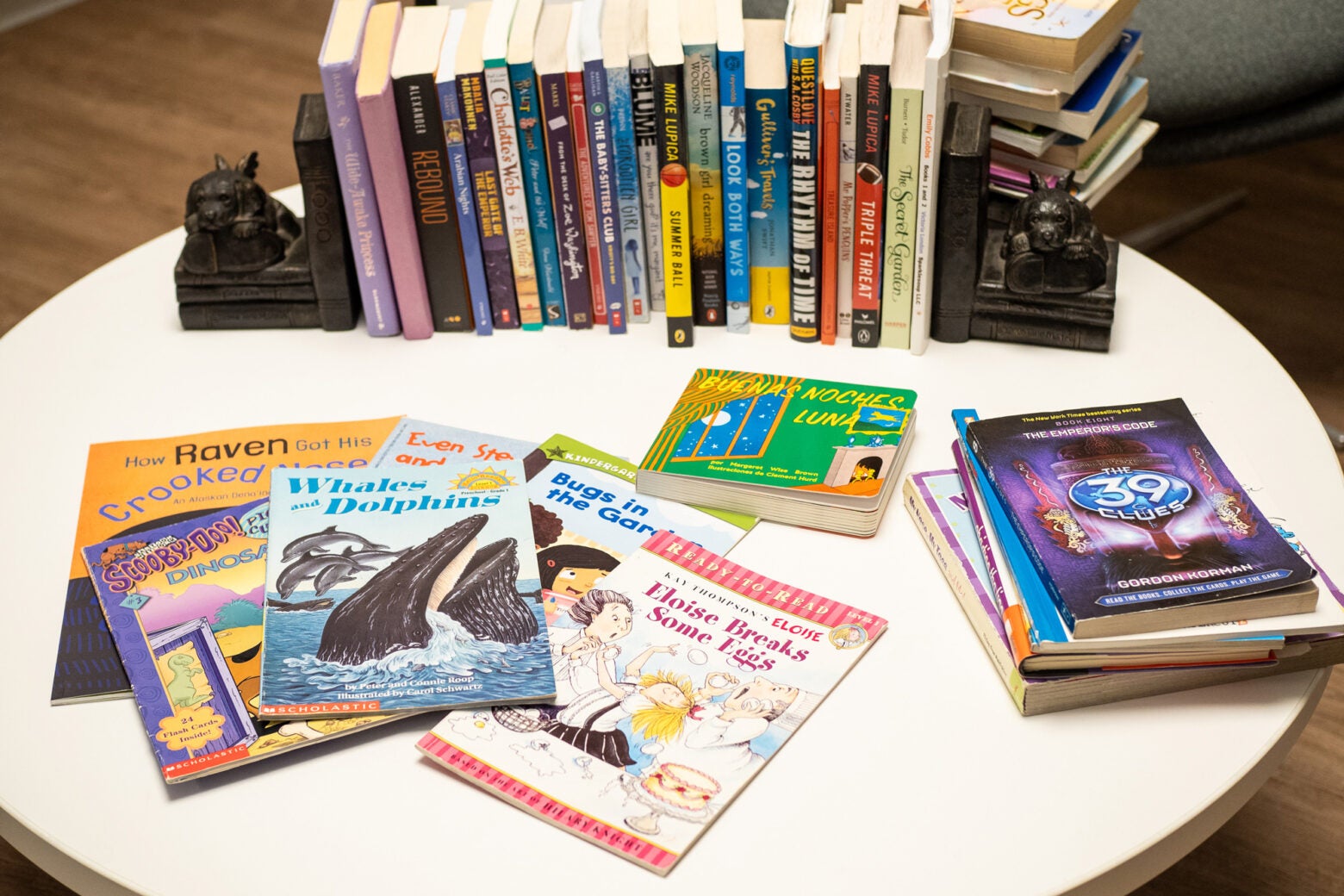
A selection of children’s books at the Yale Child Study Center, which connects families with behavioral and legal support.
Yunuen Bonaparte for The Hechinger Report
The children’s library at the Yale Child Study Center in New Haven, Connecticut. The center houses the first medical-legal partnership focused on children’s behavioral health.
Yunuen Bonaparte for The Hechinger Report
“When families come in, they tell us about struggles that might be adding stress and impacting their functioning, which could result in anxiety or depression,” said Christy Mills, a licensed clinical social worker and an associate clinical director at the Yale center. Especially since COVID, she says those struggles have increasingly included “school climate issues,” like a student’s experience of bullying and classroom challenges, both of which could lead to school avoidance.
The post-COVID data shows that New Haven is far from alone. One study quoted in a White House report found that the number of chronically absent public school students nearly doubled, from around 15 percent in the 2018-19 school year to around 30 percent in 2021-22.
Another survey focused on students with disabilities experiencing “school refusal”—a behavioral pattern describing problems with attending or staying at school—revealed 57 percent of these students had no symptoms prior to the pandemic. And for students who do attend school, their behavior struggles have increased, too; a national report of public schools in 2021-22 found more than 80 percent agreed that the pandemic negatively affected their students’ socioemotional and behavioral development. A recent study found that depression, anxiety, and suicidal thoughts in teen girls has reached record highs, and that the number of mental health hospitalizations for children more than doubled between 2016 and 2022.
Meanwhile, as children’s behavioral health struggles grow, the usual supports can’t keep up. The demand for child and adolescent psychiatrists and behavioral health providers continues to outpace supply, especially for young people already facing inequitable access to care. One estimate found that nationally, there was just one school psychologist for every 1,127 students from kindergarten to 12th grade in the 2021-22 year.
And teachers want more support, too. A recent survey of U.S. teachers found that nine in 10 reported they need more resources to care for their students’ mental health.
“Educators are doing the very best they can, but most of the time, in advocating for our low-income families, the issue cited is due to school district resources,” said Kathryn Meyer, an attorney at the Center for Children’s Advocacy, the legal partner of the Yale center.
That’s where the medical-legal team can help, by letting the school know how a child’s experience is affecting their behavior—and to connect the child’s needs to their legal rights, Meyer said. “Sometimes we’re just trying to get the student an [individualized education program, or IEP], and then, if we have the IEP, we’re trying to increase the service, or make sure that whatever is on the IEP is actually happening,” she said.

Kathryn Meyer, left, attorney at the Center for Children’s Advocacy, and Christiana Mills, are part of the Yale Child Student Center in New Haven, Connecticut. Meyer said much of her role is explaining to families the legal options that exist to help them.
Yunuen Bonaparte for The Hechinger Report
In Antonio’s case, after joining Marquez at school meetings, the medical-legal team pushed for the school to conduct another IEP evaluation, which revealed a key part of his story: Though an earlier evaluation diagnosed Antonio with attention-deficit hyperactivity disorder, the second evaluation found he had an intellectual disability as well. And once the team made the legal case that the current school couldn’t address the services his IEP mandated, Antonio was placed in a school that could.
“In moving him, our goal was to have his academic needs addressed, emotional support to keep him safe, and a smaller structure so people could really have the time to work with him,” Meyer explained.
Sure enough, that worked. According to his mother, the new school didn’t just help Antonio improve in the classroom; it improved his behavioral health, too. “Being in a place that understood him for his differences relieved a lot of his pressure and stress,” said Mills, the Yale center associate clinical director.
Antonio now spends his days outside of his room, riding bikes with his new friends or hanging out with his new girlfriend, whom he just took to prom.
“Finally, it’s like, he’s free,” his mother said. “That was the Antonio I wanted to see all these years.”
As word of the medical-legal partnership model spreads in Connecticut, educators are taking note, too. “As a former Bridgeport public school superintendent, I know just how valuable educational advocates can be for our families,” said Fran Rabinowitz, the executive director of the Connecticut Association of Public School Superintendents. “Despite districts doing our best with the limited resources we have, it’s important that we continue to elevate the voice of families, and advocacy can provide a vehicle for that voice.”
Barry Zuckerman, a pediatrician who created the first medical-legal partnership in Boston more than 30 years ago, saw the need for family advocacy first hand during his childhood, in the 1950s. He grew up with a younger brother with “significant disabilities.” But 60 years ago, Barry says, there were virtually no laws, resources or community services that could support him. His brother was eventually placed in an institution.
“Imagine a parent sending away their eight-year-old who’s never been on his own,” Zuckerman said. “It was extraordinarily traumatic for all of us.”
By the 1970s, the United States passed laws requiring schools to identify and evaluate students with disabilities, and provide them with “free, appropriate public education” tailored to their needs through individualized education programs. But Zuckerman, by then a pediatrician, realized that vulnerable families also needed support to enforce these protective laws.
In 1993, he discovered that need on the job, at Boston Medical Center, through a group of asthmatic patients. When the patients kept returning to the hospital with no improvement, Zuckerman learned that all of their homes had mold, which can trigger asthma attacks. The landlords didn’t respond to the families or to Zuckerman when they asked for mold remediation. But they did remove the mold after a lawyer friend of Zuckerman’s called.
That case would become the first of many medical-legal partnership success stories, in a model that’s expanded to over 450 health care organizations around the nation. One randomized trial found that families referred to legal support through the partnership had fewer emergency room visits six months later. Another found that patients given legal interventions had less asthma symptom severity and took fewer medications. A more recent study of a hospital in Cincinnati found that the medical-legal partnership reduced all-cause hospitalizations of children by 38 percent over five years.
Most evidence around medical-legal partnerships comes from models in primary health care. But those models have demonstrated behavioral health benefits, too. “When parents have concerns about their children’s mental health, the first place they turn is their pediatrician,” said Josh Greenberg, one of the founding medical-legal partnership lawyers in Boston.
One of Greenberg’s earliest success stories came while shadowing a seven-year-old boy during a well checkup. He learned that the boy had been out of school for six months, suspended after pushing his teacher. “The school just sent the child home and then never followed up, and never offered anything in the way of their legal rights around expulsions,” he said.
By “prescribing” legal support the same way they prescribe other kinds of medicine, health workers can see the benefits in their patients just the same. “When you have a life that’s full of stress, you can only do a few things as a doctor, but the lawyer was helping them achieve something they needed,” Zuckerman said. It also helps to level the playing field. Before, “if a child wasn’t getting their developmental needs met, many schools would blow them off, and well-to-do people got their own lawyers,” he said.
But even with the new federal funding and nationwide expansion, the number of patients who need legal support far outnumbers the supply of lawyers who can provide it, Greenberg cautioned.
That’s one reason why legal professionals are also spreading their knowledge through training and educational resources, and are reserving formal representation for extreme cases. Through the Yale partnership, for instance, of 120 patient referrals made in the program’s first year, just 20 cases went to full representation.
Instead, most of the Yale legal team’s work is focused on educating clinicians, psychiatrists, social workers and families about legal options that exist for children, and that they can access on their own. “Sometimes it’s just like, ‘Go to this place,’ or ‘call this hotline’—it’s really as simple as that,” Meyer said.
Through those trainings, clinicians can ask the legal professionals questions, too. “Sometimes we need help knowing, is this a fair legal ask? Does a family or child actually have a right to this expectation, or do we need to think about this in a different lens?” said Mills, the Yale associate clinical director.
Outside of the formal medical-legal partnership model, other organizations, like the Council for Parent Attorneys and Advocates—a national nonprofit working to protect the legal and civil rights of students with disabilities—have been similarly addressing families about their options. Selene Almazan, their legal director, said that these kinds of trainings can help prevent behavioral health struggles before they develop, especially when a student has more than one disability.
“The more information you have, the more that you know how to take care of yourself and advocate for yourself in a school setting,” Almazan said.
In her organization’s work, training parents and students on their rights has been “transformative” for students’ mental health and self-esteem. And in cases where students would otherwise be punished, Almazan says, the advocacy can completely change the trajectory of a child’s health and life.
“When kids are traumatized by exclusionary discipline or restraint and seclusion in schools, that can cause them to act out and can exacerbate any kind of mental health issues that they may already have,” she said. “Getting students what they need in school can break a pattern of family trauma and generational trauma and prevent the school-to-prison pipeline.”
Top image: SeventyFour / iStock