Feature
Researchers tried to fix a racist lung test. It got complicated.
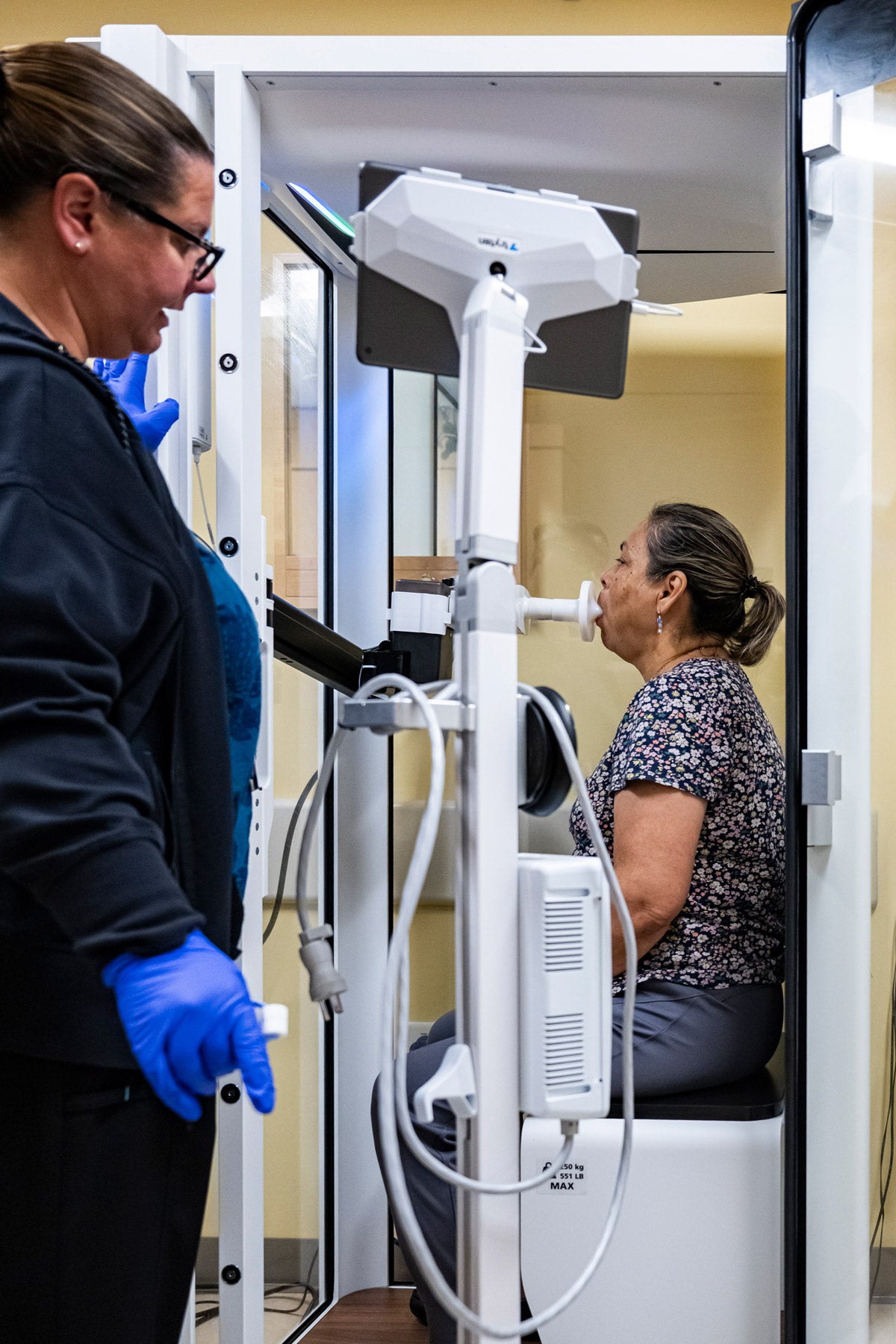
As her patient blows into a snorkel-like mouthpiece, Jennifer Winget cheers her on. “Keep going! Keep going!” she urges, voice rising all six times she says it as the patient strains to expel every last bit of air in her lungs.
Winget, a respiratory therapist at Boston Medical Center, watches a display showing an image of a pair of lungs, a bolus of air swelling within. Numbers fill a grid showing how much air the patient expelled, and how fast.
The patient, seated next to her in a glass booth, is using a device called a spirometer, which measures air flow in the lungs. It was installed in May as part of an equipment upgrade that included one especially notable change: Winget no longer has to ask patients for their race and ethnicity.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
Before, the computer program that assessed lung function sorted patients into one of four categories: Caucasian, Black, Asian, or Hispanic. It automatically lowered the threshold for what is “normal” for Black and Asian patients. It’s a startling example of how racial bias has literally been written into the machinery of 21st-century health care and how formulas based on supposed racial differences have skewed decision-making in many corners of medicine. Boston Medical Center is among the institutions working to address this problem, after an April 2023 recommendation by the American Thoracic Society that laboratories adopt a race-neutral algorithm, or set of rules, for assessments. But with thousands of lung-function laboratories and clinics scattered across the country, the movement for change faces manifold obstacles and thorny consequences.
Applying the race-neutral algorithm means broadly that Black patients will be deemed sicker and White ones healthier than before. A higher proportion of Black people (and, to a lesser extent, Asians) will be designated impaired—which could make them ineligible for certain occupations but increase their access to disability benefits, additional testing, and referral for lung transplants. White people will experience the opposite, with some potentially seeing their disability benefits reduced or eliminated.
“We can’t just change the equation without changing those downstream effects,” says Sanja Stanojevic, a Canadian pulmonary epidemiologist who co-chairs the Global Lung Function Initiative, the research collaborative that developed the new algorithmic standard. But eliminating race from the equation “is the right thing to do,” she says.

Spirometer measurements depend, to a certain extent, on how hard the patient blows into the tube. Some may try harder than others. And those measurements require interpretation. What is normal and what is a sign of illness?
Lung function varies widely among healthy people, so the machines have been programmed to compare patients to similar people with healthy lungs, based on sex, height, age—and race. Race came into the equation because of observed differences in the lungs of different racial groups. On average, Black people’s lungs tend to be smaller and to perform worse on spirometry tests.
“The problem is that no one’s ever done the work to figure out why,” says Nirav Bhakta, co-chair of the American Thoracic Society’s working group that recommended the new standard and a pulmonologist at the University of California San Francisco (UCSF). Bhakta says it was assumed that the differences were genetic. In fact, a host of factors can affect someone’s lung growth and lung function—from their mother’s nutrition while pregnant, to hazardous exposures at home and work later in life. And ample evidence shows that race is a superficial, social designation with no medical meaning; there are more differences than similarities within racial groups.

Because lower lung function was seen as “normal” for a Black person, Black patients were less likely to be diagnosed properly or treated as aggressively as White patients with a similar condition. Aaron Baugh, a pulmonary and critical care physician at UCSF and a member of the American Thoracic Society working group, recalls a worker with brown skin who came in for a disability assessment about five years ago. He was identified as Black for the spirometer, which rated his lung function as normal. But he continued to struggle with severe symptoms. When he told his doctors that one of his parents is White, they changed his race in the system. “We just reprocessed it, clicking one button from Black to White, and all of a sudden, he changed from all normal scores to some significant disability,” Baugh says. “That was a big moment of reflection for us.”
UCSF completed reprogramming its devices with a race-neutral equation in March.
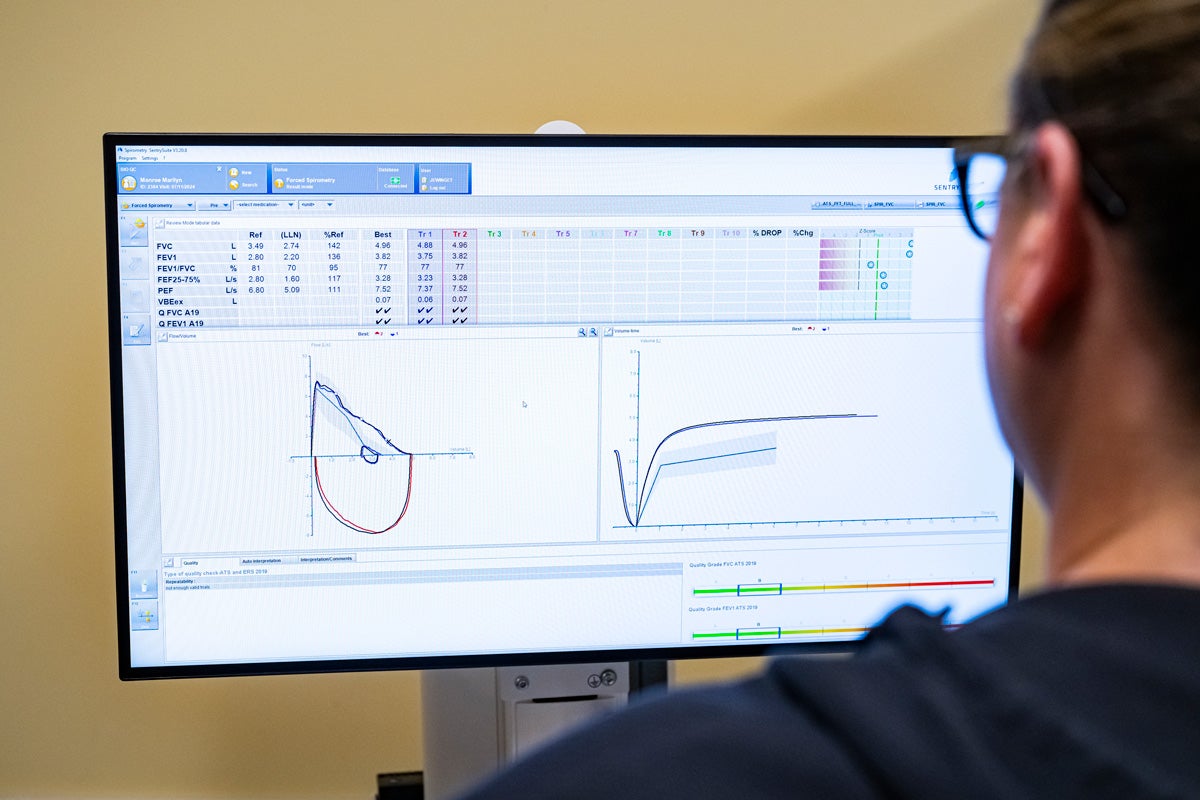
Jennifer Winget, a respiratory therapist at Boston Medical Center, displays sample lung function test results from a spirometer in July 2024.
One impetus for the changes was Lundy Braun’s 2014 book, Breathing Race into the Machine: The Surprising Career of the Spirometer. It showed how the “deficiency” of Black people’s lungs, as noted by Thomas Jefferson, became a justification for slavery and later an accepted fact. Braun found that the vast majority of studies didn’t even define “race.”
“We basically created this huge edifice of racialization of the statistics themselves, the numbers themselves, in pulmonary medicine, and without ever defining what it is we’re talking about,” Braun said in an interview earlier this year (she died in August).
Another catalyst was a paper by David S. Jones, a psychiatrist and Harvard University professor, and two of his former students at Harvard Medical School. They identified 13 tools in eight disciplines that used race-based formulas to gauge lung function, estimate the risk of osteoporosis and breast cancer, and predict the likelihood of death from heart failure. Based on research that made outdated assumptions about race, the tools “all directed medical resources towards White people, away from Black people,” Jones says.
Jones submitted his paper to the New England Journal of Medicine in early March 2020. Less than three months later, George Floyd was murdered, prompting the editors to fast-track the article for publication in June. Amid the national reckoning over race that has since ensued, organizations that developed the tools have reconsidered them and, in some cases, made revisions. In September 2021 the National Kidney Foundation and the American Society of Nephrology recommended a race-neutral calculation for estimating kidney function, resulting in more Black people becoming eligible for kidney transplants. But when the American Thoracic Society tackled the issue that same year, its working group could not reach a consensus, with concerns raised about unintended consequences and possible harm to patients. Then five research studies demonstrated that race-neutral equations yielded more accurate prognoses, and in 2023 the group decided to act, although not without dissent.
“We just reprocessed it, clicking one button from Black to White, and all of a sudden, he changed from all normal scores to some significant disability.”
Aaron Baugh, UCSF pulmonary and critical care physician
While the new standard amounted to calling for the reprogramming of every spirometer in the country, it is merely a recommendation. It is unclear how many machines have been updated. Upgrading to the new formula can be as straightforward as a software update, says Nadia Stachowicz, a senior product manager at spirometer maker Vyaire Medical (who was offering her own views and not those of her employer). Vyaire, she says, provides simple software patches for free, but labs that use outdated Windows software need a full upgrade. Some have equipment so old that the hardware must be replaced, too.
Boston Medical Center had been planning to replace its outdated equipment even before the new standard was released. The year-long project was “immense,” says Michael Ieong, medical director of the hospital’s pulmonary function laboratory, and involved integrating electronic medical records and explaining the change to an array of subspecialists who use lung-function tests in clinical decisions.
It’s not yet clear what the new standard means for patients. One recent paper estimates that as many as 12.5 million people could receive a revised diagnosis, potentially affecting clinical, employment, and insurance decisions. Some 750,000 Black people may no longer be deemed eligible to serve as firefighters, for example. Disability compensation could change for some 413,000 military veterans, with Black people gaining benefits while some White people may see theirs reduced or eliminated. Life insurance premiums could rise for Black people—as could the number considered eligible for lung transplants.
The results come with “a lot of caveats,” says James Diao, the paper’s lead author. Among them: Most people will never be tested. Others’ test results may not be relevant. “A lot of people who, for example, would not be allowed to work as firefighters have no intention of working as firefighters,” says Diao, who was a Harvard Medical School student when the study was published and recently started his residency at Brigham and Women’s Hospital in Boston.
The potential cost of disability payments and changes in who qualifies for them is a concern. Diao’s team looked at the impact on veterans and calculated that annual disability payments would increase by 17 percent, or $1.1 billion, for Black veterans and drop by about 1 percent, or more than $500 million, for White veterans.
Estimates are not available for others who may qualify for disability payments through private insurance or state programs, but observers anticipate similar effects, with Black people more likely to be diagnosed with severe illness and thus eligible for more benefits, while White people might lose disability payments. “Some people will benefit and some people will be harmed. This is all part of the pushback,” says Jones, the Harvard professor. “People are willing to do something to help Black people, but they become very alarmed if that’s at the expense of White people. . . . But it doesn’t mean that they were justly receiving these disability payments previously.”
The algorithmic change will have little effect on Social Security, which already uses a single standard for all races when determining disability from respiratory disorders.
Several doctors at laboratories using updated algorithms say that so far, they’ve seen little practical impact on patients’ diagnoses. They emphasize that, while Diao’s study focused on spirometry, lung health is assessed using multiple tests and factors.
The University of Colorado has some of the longest experience with a race-neutral algorithm, having switched in 2022 (its algorithm is similar to the new standard). Jeffrey Sippel, a critical care pulmonologist at Colorado’s Anschutz Medical Campus in Aurora, says he has not observed dramatic shifts for patients. A survey of about 250 patients found little change in eligibility for transplants, for example. And decisions about lung cancer surgery come from a multidisciplinary “tumor board” that reviews a variety of factors beyond the spirometry results. “One data point—it doesn’t really have the ability to make or break a decision like that,” Sippel says.

But that one data point can make or break a decision about whether to award disability payments, cautions Bhakta, the American Thoracic Society working group co-chair. Insurance companies and government administrators make those determinations—and they rely on a chart that sets impairment levels based solely on the pulmonary function test, he says.
Stanojevic, co-chair of the Global Lung Function Initiative, would like to see an end to such rigid categories in disability decisions. Spirometer readings are hardly objective, she notes, since they depend on how hard patients blow into the tube. “We strongly advocate for people to be treated as individuals . . . and for these cut points to be augmented with other clinical information,” she says. “How a patient feels and how a patient functions should be our first and primary focus.”
The shadow of uncertainty prompted the Veterans Health Administration, the nation’s largest health care provider, to pause its rollout in January, after it had adopted the new approach in some 30 percent of its lung-function laboratories. The decision was triggered by a 2023 study in JAMA Surgery suggesting that the new equation would make surgeons less likely to recommend lung cancer surgery to Black people. That finding was “alarming,” says David Au, a pulmonary physician who directs the Center for Care and Payment Innovation in the Department of Veterans Affairs (the VA), because the VA had labored to end racial disparities in lung cancer treatment. “Our principal concern was that we would induce new health care disparities that the organization had already resolved,” he says.
Treating lung cancer can include removing a portion of the patient’s lungs. Spirometry helps doctors determine whether the organs are strong enough to withstand the effects of the surgery. The new algorithm creates the possibility that more Black patients will be denied lung cancer surgery. But other doctors note that previously, Black patients’ lung strength may have been overestimated, leading to ill-advised surgery. Au says the VA will monitor the laboratories using the race-neutral algorithm and study the research that underlies the new standard, a process he hopes to complete by next year.
Meanwhile, at Boston Medical Center, where more than 70 percent of patients identify as people of color, Michael Ieong says it will take time to observe the effects of the new algorithm. Speaking in July, Ieong said that in the few weeks it has been in place, he has yet to encounter a patient whose status changed because of it. “The people that this is affecting are the people that are on the margin already between normal and abnormal . . . people who are right on the cusp,” Ieong says.
But Winget, the respiratory therapist, feels the difference every day: She no longer has to ask patients about their race or ethnicity. She’d always felt uncomfortable asking, and patients often didn’t know how to answer. Some said they don’t identify with any of the groups. Others gave different answers on different visits. “Some patients would get very upset with me,” Winget says.
She’s relieved the race question is gone.
Top image: Jennifer Winget, a respiratory therapist at Boston Medical Center, talks to Isabel Flores de Lopez, 62, who is using a spirometer for testing lung function in July 2024.
Headshots: Courtesy of Sanja Stanojevic, Nirav Bhakta, Jeffery Sippel and David Au. Michael Ieong: Ben Gebo


