People
Inside CRISPR’s gene editing revolution
Among the things on Jennifer Doudna’s Nobel Prize-winning mind are cow farts. Cows’ digestive processes release methane, and there are enough cows in the world that their natural gas is a major contributor to climate change. Doudna is working to genetically alter the microbiome of cows to produce less methane. It’s work made possible by the gene editing technology known as CRISPR, for which she shared the 2020 Nobel Prize in Chemistry. CRISPR uses a specific protein like a pair of scissors to splice genetic code, which Doudna describes as “a surgical tool at the molecular level”—one so precise, “we can alter a single letter of the DNA code in a cell.”
CRISPR now has dozens of approved and experimental applications. Besides making cows safer for the planet, Doudna’s also jazzed about bananas that never brown (now on sale in Japan), cattle without horns (not just yet), and innovations in research on Alzheimer’s and asthma.
And of course, there’s curing sickle cell anemia, perhaps CRISPR’s best-known application. Last year, the sickle cell treatment known as Casgevy became the first FDA-approved CRISPR therapy. “Who could have imagined that in just 10 years, we would get to an approved therapeutic with the very same molecule that we had studied academically?” Doudna says.
The speed of CRISPR’s development and the risks and ethical concerns raised by such technological advances were part of Doudna’s conversation with Alice Park, TIME magazine’s senior health correspondent, at Aspen Ideas: Health, a three-day annual event in that idyllic town. Their hour-long discussion has been condensed and edited for Harvard Public Health by HPH editor Jina Moore Ngarambe.
Park: CRISPR is a double-edged sword. For scientists it’s relatively easy, technology-wise, and it can be used for nefarious purposes. How did you initially think about unleashing this technology to the world, and how has your thinking around that changed?
Doudna: I remember being at a dinner at my house with some neighbors. One of them, a computer scientist . . . said, “Wait a minute, you mean you could put that in somebody’s body and it could manipulate any of their genes?”
Not too long after that, a paper was published in a scientific journal in which a team reported that they were using CRISPR in monkey embryos to make germline changes, heritable changes, to DNA, and those edited embryos were implanted—monkeys were born with these heritable changes. And when I read that paper, I thought, “You know, there’s no technical reason why this couldn’t happen in humans.” And that was really for me that moment when I realized, okay, I have to get out of the lab and start talking about this because it’s such a powerful tool. Humans now have a tool that can basically change who we are.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
Park: You’ve talked about how, as a scientist, you didn’t feel initially fully equipped to address those ethical, social, and cultural concerns. How did that change as the years went by?
Doudna: I definitely didn’t. So I called two people [Paul Berg and David Baltimore] that actually had been at the forefront of an earlier iteration of ethical grappling in the 1970s, when the technology for manipulating bacteria came along. Scientists realized similarly that there could be real risk in manipulating the bacteria that populate our bodies, for example. Both of them were incredibly helpful in the CRISPR community and helping people like me to get our heads around what was coming with the technology, how to think about it, and how to initiate a more open discussion about it.
Park: And the things that they did around that technology, you modeled a lot of that around CRISPR—in terms of having a scientific community adopt a voluntary moratorium on certain applications of it in human embryos, for example.
Doudna: Right. I think that really started a whole movement in the field, in and among scientists, to get together and figure out how we were going to collectively manage a very powerful technology. We published a paper about it with the discussion of a moratorium, [and] we started being contacted by government agencies and regulators in different countries.
Park: Despite those best intentions, of course, in 2018, a Chinese scientist announced that he had actually done the worst case scenario and had used CRISPR to edit embryos that were then implanted, resulted in the birth of twin girls. Tell me about how you learned about that and the steps that you took immediately afterwards.
Doudna: I learned about that right before a conference that I was one of the co-organizers [of], that was being held in Hong Kong to discuss this very topic of human germline editing: Should we do it? How do we manage it? How do we control the technology? And this scientist got in touch and said, “Well, I’ve done this,” and sent me a manuscript that he had drafted about the work.
He was already scheduled to speak at the conference, so our decision among the conference organizers was, let’s have him come and present his work and open it up for questions.
It was a bit horrifying to hear what had been done. It really sounded unethical. There was an initial buzz around the work, but I think very quickly people realized that this isn’t something that should be happening right now. The technology’s not advanced enough to do it safely. And even if it was, we haven’t had the opportunity as a community to figure out when and how should germline editing happen with something like CRISPR. That scientist was actually punished; he was ultimately jailed for that work. So that was like a real wake-up call.
Park: Currently the sickle cell treatment, as exciting as it is, I think the current price is about $2.2 million, which seems like a lot—but if you consider the kind of accrued cost of what patients pay throughout their lifetime for transfusions and other treatments, it could be a cost savings, ultimately. You’re addressing this affordability issue and finding ways to also make it more accessible, especially in the clinical space. Can you tell us about some of the ways that CRISPR could potentially be[come] easier to do at more healthcare facilities, or for more providers to do?
Doudna: Well, let’s start with what you said about CRISPR being a therapy that is kind of different than a traditional therapeutic. Because [for sickle cell] it’s really a one-and-done treatment. When you give this treatment to patients once, they are effectively cured of their symptoms. And so if that is really true for something like sickle cell, you could argue that a price tag like the current one is, you know—maybe it actually makes financial sense when you look at the cost of care for patients over their lifetime.
On the other hand, it’s a cost price point that absolutely won’t work for the vast majority of people, both in this country and globally. And that’s something that I think is not right. We need to address that. So we’re working hard at our institute on ways to reduce the cost and make it much more affordable.
One of the big technical advances that we’re working hard on [in an ongoing phase I clinical trial] is to make it possible to introduce the CRISPR molecules without requiring a bone marrow transplant for patients. That would make it much, much easier to give this therapy to people, and make it easier for manufacturing as well.
Park: [The sickle cell treatment] also requires chemo[therapy] now, right?
Doudna: Exactly, yeah. Which is also very invasive, and it’s very unpleasant for patients. So I think there’s a real opportunity, as exciting as it is to see this [current treatment], to make it even better.
Park: Looking ahead, what application of CRISPR are you most excited to see come into fruition?
Doudna: I’m really, really excited about this work we’re doing [with] the microbiome. We’re also working with a team at UC San Francisco where we’re hoping to manipulate the human gut microbiome to reduce production of molecules that make children more susceptible to asthma. And if that approach works with asthma, you could imagine impacting the microbiome in other ways. We’re just at the beginning of understanding how the microbiome affects our health in so many ways. And I think that having a technology that can allow us to manipulate that set of organisms that are so integral to our health is gonna be really powerful.
To hear Doudna discuss the rapidly growing agricultural uses of CRISPR, some early work toward using CRISPR for Alzheimer’s research, and her regrets about how intellectual property disputes have hampered some research, listen to the full conversation at Aspen Ideas: Health.
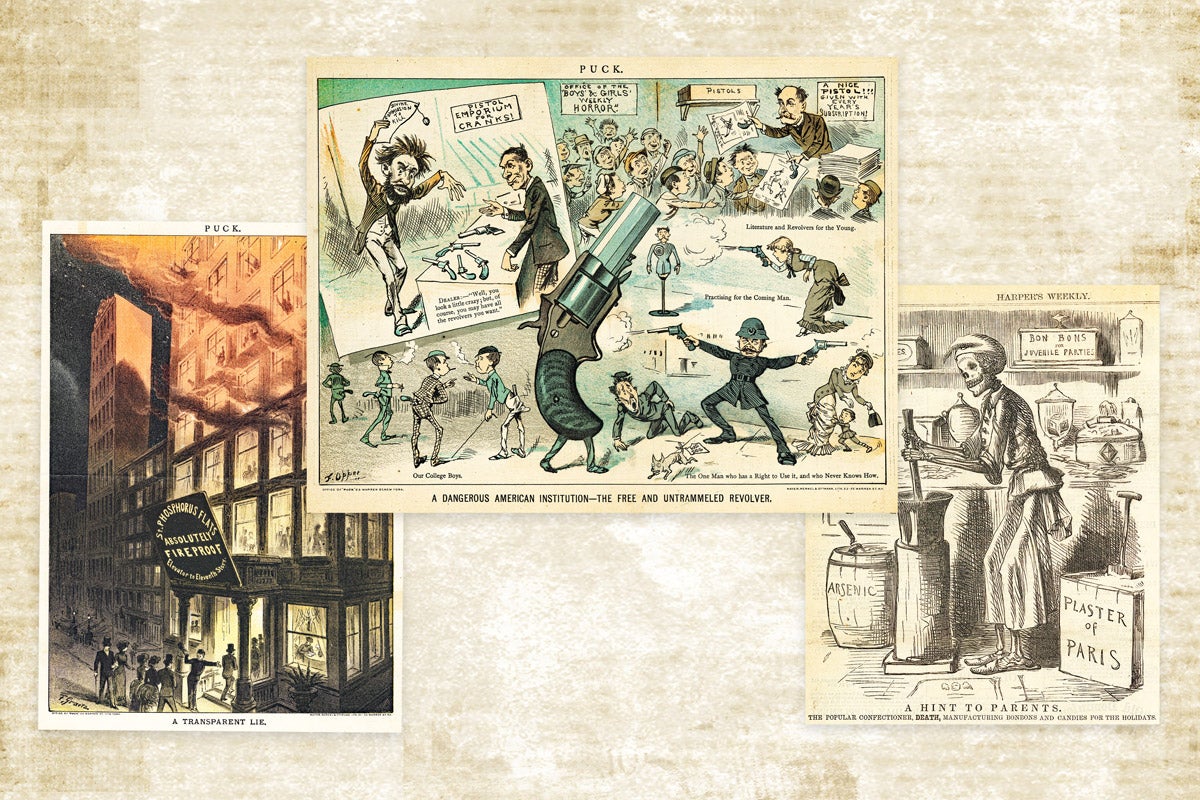
Lead image: Alice Park and Jennifer Doudna seated on stage for a session talk at Aspen Ideas: Health. (Nick Tininenko / Aspen Ideas: Health)
Republish this article
<p>Jennifer Doudna won the Nobel Prize for inventing a powerful gene editing technology. What comes next for CRISPR?</p>
<p>Written by Jina Moore Ngarambe</p>
<p>This <a rel="canonical" href="https://harvardpublichealth.org/tech-innovation/inside-crisprs-gene-editing-revolution/">article</a> originally appeared in<a href="https://harvardpublichealth.org/">Harvard Public Health magazine</a>. Subscribe to their <a href="https://harvardpublichealth.org/subscribe/">newsletter</a>.</p>
<p class="has-drop-cap">Among the things on Jennifer Doudna’s Nobel Prize-winning mind are cow farts. Cows' digestive processes release methane, and there are enough cows in the world that their natural gas is a major <a href="https://climate.ec.europa.eu/climate-change/causes-climate-change_en">contributor</a> to climate change. Doudna is working to genetically <a href="https://www.ucdavis.edu/food/news/can-crispr-cut-methane-emissions-cow-guts">alter the microbiome</a> of cows to produce less methane. It’s work made possible by the gene editing technology known as CRISPR, for which she shared the 2020 Nobel Prize in Chemistry. CRISPR uses a specific protein like a pair of scissors to splice genetic code, which Doudna describes as “a surgical tool at the molecular level”—one so precise, “we can alter a single letter of the DNA code in a cell.”</p>
<p>CRISPR now has dozens of approved and experimental applications. Besides making cows safer for the planet, Doudna’s also jazzed about bananas that never brown (now on sale in Japan), cattle without horns (not just yet), and innovations in research on Alzheimer’s and asthma.</p>
<p>And of course, there’s <a href="https://innovativegenomics.org/news/crispr-clinical-trials-2024/" target="_blank" rel="noreferrer noopener">curing</a> sickle cell anemia, perhaps CRISPR’s best-known application. Last year, the sickle cell treatment known as Casgevy became the <a href="https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease" target="_blank" rel="noreferrer noopener">first FDA-approved</a> CRISPR therapy. “Who could have imagined that in just 10 years, we would get to an approved therapeutic with the very same molecule that we had studied academically?” Doudna says.</p>
<p>The speed of CRISPR’s development and the risks and ethical concerns raised by such technological advances were part of Doudna's conversation with Alice Park, <em>TIME</em> magazine’s senior health correspondent, at <a href="https://www.aspenideas.org/attend/health" target="_blank" rel="noreferrer noopener">Aspen Ideas: Health</a>, a three-day annual event in that idyllic town. Their hour-long discussion has been condensed and edited for <em>Harvard Public Health</em> by HPH editor Jina Moore Ngarambe.</p>
<p><strong>Park</strong>: CRISPR is a double-edged sword. For scientists it's relatively easy, technology-wise, and it can be used for nefarious purposes. How did you initially think about unleashing this technology to the world, and how has your thinking around that changed?</p>
<p><strong>Doudna: </strong>I remember being at a dinner at my house with some neighbors. One of them, a computer scientist . . . said, “Wait a minute, you mean you could put that in somebody's body and it could manipulate any of their genes?”</p>
<p>Not too long after that, a paper was published in a scientific journal in which a team reported that they were using CRISPR in monkey embryos to make germline changes, heritable changes, to DNA, and those edited embryos were implanted—monkeys were born with these heritable changes. And when I read that paper, I thought, “You know, there's no technical reason why this couldn't happen in humans.” And that was really for me that moment when I realized, okay, I have to get out of the lab and start talking about this because it's such a powerful tool. Humans now have a tool that can basically change who we are.</p>
<p><strong>Park</strong>: You’ve talked about how, as a scientist, you didn't feel initially fully equipped to address those ethical, social, and cultural concerns. How did that change as the years went by?</p>
<p><strong>Doudna</strong>: I definitely didn't. So I called two people [<a href="https://www.science.org/doi/10.1126/science.adh2943">Paul Berg</a> and <a href="https://www.science.org/doi/10.1126/science.adh2943">David Baltimore</a>] that actually had been at the forefront of an earlier iteration of ethical grappling in the 1970s, when the technology for manipulating bacteria came along. Scientists realized similarly that there could be real risk in manipulating the bacteria that populate our bodies, for example. Both of them were incredibly helpful in the CRISPR community and helping people like me to get our heads around what was coming with the technology, how to think about it, and how to initiate a more open discussion about it.</p>
<p><strong>Park</strong>: And the things that they did around that technology, you modeled a lot of that around CRISPR—in terms of having a scientific community adopt a voluntary moratorium on certain applications of it in human embryos, for example.</p>
<p><strong>Doudna</strong>: Right. I think that really started a whole movement in the field, in and among scientists, to get together and figure out how we were going to collectively manage a very powerful technology. We published a paper about it with the discussion of a moratorium, [and] we started being contacted by government agencies and regulators in different countries.</p>
<p><strong>Park</strong>: Despite those best intentions, of course, in 2018, a Chinese scientist announced that he had actually done the worst case scenario and had used CRISPR to edit embryos that were then implanted, resulted in the birth of twin girls. Tell me about how you learned about that and the steps that you took immediately afterwards.</p>
<p><strong>Doudna</strong>: I learned about that right before a conference that I was one of the co-organizers [of], that was being held in Hong Kong to discuss this very topic of human germline editing: Should we do it? How do we manage it? How do we control the technology? And this scientist got in touch and said, "Well, I've done this," and sent me a manuscript that he had drafted about the work.</p>
<p>He was already scheduled to speak at the conference, so our decision among the conference organizers was, let's have him come and present his work and open it up for questions.</p>
<p>It was a bit horrifying to hear what had been done. It really sounded unethical. There was an initial buzz around the work, but I think very quickly people realized that this isn't something that should be happening right now. The technology's not advanced enough to do it safely. And even if it was, we haven't had the opportunity as a community to figure out when and how should germline editing happen with something like CRISPR. That scientist was actually punished; he was ultimately jailed for that work. So that was like a real wake-up call.</p>
<p><strong>Park</strong>: Currently the sickle cell treatment, as exciting as it is, I think the current price is about $2.2 million, which seems like a lot—but if you consider the kind of accrued cost of what patients pay throughout their lifetime for transfusions and other treatments, it could be a cost savings, ultimately. You're addressing this affordability issue and finding ways to also make it more accessible, especially in the clinical space. Can you tell us about some of the ways that CRISPR could potentially be[come] easier to do at more healthcare facilities, or for more providers to do?</p>
<p><strong>Doudna</strong>: Well, let's start with what you said about CRISPR being a therapy that is kind of different than a traditional therapeutic. Because [for sickle cell] it's really a one-and-done treatment. When you give this treatment to patients once, they are effectively cured of their symptoms. And so if that is really true for something like sickle cell, you could argue that a price tag like the current one is, you know—maybe it actually makes financial sense when you look at the cost of care for patients over their lifetime.</p>
<p>On the other hand, it's a cost price point that absolutely won't work for the vast majority of people, both in this country and globally. And that's something that I think is not right. We need to address that. So we're working hard at our institute on ways to reduce the cost and make it much more affordable.</p>
<p>One of the big technical advances that we're working hard on [in an ongoing phase I clinical trial] is to make it possible to introduce the CRISPR molecules without requiring a bone marrow transplant for patients. That would make it much, much easier to give this therapy to people, and make it easier for manufacturing as well.</p>
<p><strong>Park</strong>: [The sickle cell treatment] also requires chemo[therapy] now, right?</p>
<p><strong>Doudna</strong>: Exactly, yeah. Which is also very invasive, and it's very unpleasant for patients. So I think there's a real opportunity, as exciting as it is to see this [current treatment], to make it even better.</p>
<p><strong>Park</strong>: Looking ahead, what application of CRISPR are you most excited to see come into fruition?</p>
<p class=" t-has-endmark t-has-endmark"><strong>Doudna</strong>: I'm really, really excited about this work we're doing [with] the microbiome. We're also working with a team at UC San Francisco where we're hoping to manipulate the human gut microbiome to reduce production of molecules that make children more susceptible to asthma. And if that approach works with asthma, you could imagine impacting the microbiome in other ways. We're just at the beginning of understanding how the microbiome affects our health in so many ways. And I think that having a technology that can allow us to manipulate that set of organisms that are so integral to our health is gonna be really powerful.</p>
<p class="is-style-t-caption"><em>To hear Doudna discuss the rapidly growing agricultural uses of CRISPR, some early work toward using CRISPR for Alzheimer’s research, and her regrets about how intellectual property disputes have hampered some research, </em><a href="https://www.aspenideas.org/sessions/in-conversation-with-crispr-pioneer-jennifer-doudna" target="_blank" rel="noreferrer noopener"><em>listen to the full conversation at Aspen Ideas: Health</em></a><em>.</em></p>
<script async src="https://www.googletagmanager.com/gtag/js?id=G-S1L5BS4DJN"></script>
<script>
window.dataLayer = window.dataLayer || [];
if (typeof gtag !== "function") {function gtag(){dataLayer.push(arguments);}}
gtag('js', new Date());
gtag('config', 'G-S1L5BS4DJN');
</script>
Republishing guidelines
We’re happy to know you’re interested in republishing one of our stories. Please follow the guidelines below, adapted from other sites, primarily ProPublica’s Steal Our Stories guidelines (we didn’t steal all of its republishing guidelines, but we stole a lot of them). We also borrowed from Undark and KFF Health News.
Timeframe: Most stories and opinion pieces on our site can be republished within 90 days of posting. An article is available for republishing if our “Republish” button appears next to the story. We follow the Creative Commons noncommercial no-derivatives license.
When republishing a Harvard Public Health story, please follow these rules and use the required acknowledgments:
- Do not edit our stories, except to reflect changes in time (for instance, “last week” may replace “yesterday”), make style updates (we use serial commas; you may choose not to), and location (we spell out state names; you may choose not to).
- Include the author’s byline.
- Include text at the top of the story that says, “This article was originally published by Harvard Public Health. You must link the words “Harvard Public Health” to the story’s original/canonical URL.
- You must preserve the links in our stories, including our newsletter sign-up language and link.
- You must use our analytics tag: a single pixel and a snippet of HTML code that allows us to monitor our story’s traffic on your site. If you utilize our “Republish” link, the code will be automatically appended at the end of the article. It occupies minimal space and will be enclosed within a standard <script> tag.
- You must set the canonical link to the original Harvard Public Health URL or otherwise ensure that canonical tags are properly implemented to indicate that HPH is the original source of the content. For more information about canonical metadata, click here.
Packaging: Feel free to use our headline and deck or to craft your own headlines, subheads, and other material.
Art: You may republish editorial cartoons and photographs on stories with the “Republish” button. For illustrations or articles without the “Republish” button, please reach out to republishing@hsph.harvard.edu.
Exceptions: Stories that do not include a Republish button are either exclusive to us or governed by another collaborative agreement. Please reach out directly to the author, photographer, illustrator, or other named contributor for permission to reprint work that does not include our Republish button. Please do the same for stories published more than 90 days previously. If you have any questions, contact us at republishing@hsph.harvard.edu.
Translations: If you would like to translate our story into another language, please contact us first at republishing@hsph.harvard.edu.
Ads: It’s okay to put our stories on pages with ads, but not ads specifically sold against our stories. You can’t state or imply that donations to your organization support Harvard Public Health.
Responsibilities and restrictions: You have no rights to sell, license, syndicate, or otherwise represent yourself as the authorized owner of our material to any third parties. This means that you cannot actively publish or submit our work for syndication to third-party platforms or apps like Apple News or Google News. Harvard Public Health recognizes that publishers cannot fully control when certain third parties aggregate or crawl content from publishers’ own sites.
You may not republish our material wholesale or automatically; you need to select stories to be republished individually.
You may not use our work to populate a website designed to improve rankings on search engines or solely to gain revenue from network-based advertisements.
Any website on which our stories appear must include a prominent and effective way to contact the editorial team at the publication.
Social media: If your publication shares republished stories on social media, we welcome a tag. We are @PublicHealthMag on X, Threads, and Instagram, and Harvard Public Health magazine on Facebook and LinkedIn.
Questions: If you have other questions, email us at republishing@hsph.harvard.edu.