Feature
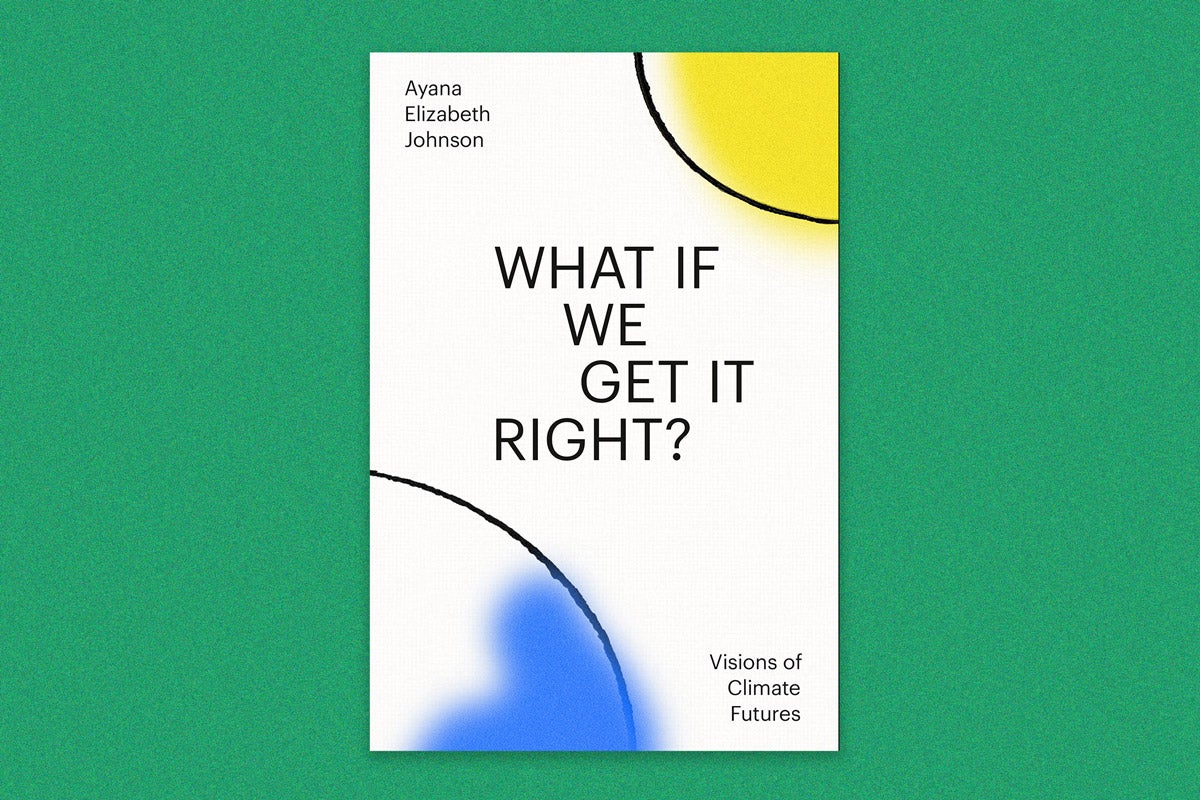
No time to waste
The world is waking up to the totality of climate change. For years, rising carbon dioxide emissions, melting ice caps, and warming oceans have largely been framed as an environmental problem. But now, we’re seeing in real time how these converging crises undercut public health and threaten the lives of millions of people. Intense weather events disrupt access to health care and can result in acute and long-term health threats. Heat-related deaths have soared globally in the last two decades. Air pollution from wildfires, which are increasing in frequency and intensity, strains the lungs of already vulnerable populations around the world, from San Francisco to Sri Lanka.
The pages that follow highlight some of the many ways in which scientists from across departments and research centers at the Harvard T.H. Chan School of Public Health are working collectively to meet the challenge of climate change. Their efforts—whether it’s analyzing the intersection of racial justice and CO2 emissions or creating models to determine where renewable energy will have the greatest public health impact—are changing how we think about climate change and how we respond to it. As many of them pointed out, efforts to counter climate change are often “benefit multipliers”: Reduce carbon emissions and air pollution, and you’ll reduce the burden of asthma and heart disease. Build resilient and equitable health systems, and everyone will fare better in the face of a historic storm.
Now, they say, it’s time to act.
Sign up for Harvard Public Health
Delivered to your inbox weekly.
Equity & Environment
Fight climate change, fight inequity
In the push to close health disparities and build stronger communities, climate action could be one of our most powerful tools, says Harvard Chan C-CHANGE Yerby Fellow Renee Salas.
As a physician, how do you think about the threats climate change poses to already vulnerable populations?

Renee Salas: The simple truth is that we cannot tackle health disparities stemming from structural racism without action on climate change, as we recently outlined in the 2020 Lancet Countdown on Health and Climate Change Brief for the United States. Climate change and air pollution are also interconnected, as they have the same root cause: the burning of fossil fuels.
Three key aspects of vulnerability are susceptibility, exposure, and the ability to adapt. For example, individuals who are Black, Indigenous, or people of color (BIPOC) can be more likely to suffer from asthma due to higher air pollution exposure by living closer to power plants and highways. As asthma heightens their susceptibility, they are more vulnerable to other climate-related exposures, such as living in hotter areas of a city called urban heat islands. Those who are BIPOC are then also at a disadvantage in their ability to adapt to these threats. For example, a recent report from the Agency for Healthcare Research and Quality found consistent disparities for some people who are BIPOC, as they received worse care than white individuals on approximately 40 percent of the quality measures.
What’s important to recognize is that policy decisions have helped create these disparities. Thus, we can craft deliberate policies that target these vulnerabilities and remedy multiple crises—climate change, air pollution, and inequitable health care quality—all at once. Actions like replacing the burning of fossil fuels with zero-carbon solutions that will reduce air pollution in the near term, adapting a city’s infrastructure to reduce heat exposure, and implementing health policies that address inequitable quality measures will all push us in the right direction.
Are our health systems appropriately adapting to climate change?
Salas: We can no longer use a rearview mirror to understand what challenges our health care systems will face from climate change in the future. After a severe winter storm hit Texas in February, we saw disruptions to power and water that jeopardized the delivery of care and forced some health care facilities to evacuate patients. When Hurricane Maria hit Puerto Rico in 2017, we saw dire shortages of saline solution. There are dozens of recent examples.
There’s an enormous opportunity for us to increase the resilience and adaptability of our hospital infrastructure, power grids, and supply chains. In doing so, it’s really critical to understand local vulnerabilities and work closely with surrounding health systems within a city or a region to synergize interventions. And this is where I think the federal government has an opportunity to play an essential role in coordinating and supporting hospital preparedness.
What else needs to be done to understand how climate change is impacting health and health care delivery?
Salas: Broadly speaking, we need a multidisciplinary approach that makes health and health equity central to climate action and all policy decisions. A key piece to achieve this goal is research and surveillance that allows us to build an evidence-based path forward so that we can optimally prepare. In addition to expanding current research collaborations, we need to optimize existing infrastructure and focus a climate lens on domestic health policy. One recommendation is to create a real-time national surveillance system for climate-related health exposures and health care delivery disruptions. We can then start to better understand the cascading failures, how these crises converge, and what populations and communities are most impacted. This will, in turn, allow us to target adaptation and resiliency actions for the communities that are most harmed.
You recently told the New York Times that “climate action is a prescription for health.” Can you elaborate?
Salas: When a patient is rushed to my emergency department, our care is guided by three core tenets: teamwork, parallel actions, and timely intervention. A diverse team works together to save the person’s life, oftentimes implementing numerous interventions within a critical window. If we hold back treatments or give them too late, they may not be as effective or even work at all. In my opinion, climate action fits these same three tenets. We need to work as a team to take parallel actions so that we can simultaneously protect health from the harms of climate change. And we need to act now in this critical window of time, because if we delay or withhold actions, we may pass the point of no return.
Unequal impact
For disadvantaged populations in the U.S., climate change may make a bad situation worse.
1.8m
Latinos in the U.S. who live within a half-mile radius of oil and gas developments
86
percent of Alaska Native villages that are now threatened by erosion and flooding
2x
increased likelihood that an African American living in Los Angeles will die during a heat wave compared with other residents of the city
98
percent decline in the amount of surface water flowing in streams on the Navajo Nation during the 20th century, which has been attributed to increasing temperatures and declining precipitation
3x
increased likelihood an African American will die from or visit the emergency department for asthma-related complications compared with the non-Hispanic white population
Sources: Climatic Change; National Hispanic Medical Association; Government Accountability Office; U.S. Department of Health and Human Services Office of Minority Health; U.S. Water Alliance
Seed idea
Climate action is racial justice
Whenever Gaurab Basu thinks about a big problem, he thinks about history. Ask him about climate change, and he sketches the history of redlining, the New Deal–era federal policy that encouraged banks not to invest in communities of color—which were predominantly in urban areas—while underwriting mortgages for white families. Today, research shows that formerly redlined neighborhoods are on average 2.6 degrees Celsius hotter than nonredlined neighborhoods in the U.S., and sometimes the difference is as much as 7 degrees Celsius.
“Redlining is a great example of where we have offered structured opportunity for some and taken it away from others,” says Basu, a health equity fellow at Harvard Chan C-CHANGE (Center for Climate, Health, and the Global Environment) and a primary care physician with Cambridge Health Alliance. “And climate change follows those same fault lines of injustice. The racist principles that enabled redlining are the same principles that enable communities of color to be significantly and disproportionally harmed by the impacts of fossil fuel infrastructure.”
In that context, Basu explains, actions to counter climate change in lower-income communities and communities of color—whether it’s creating new green space or improving access to public transit—are inherently acts of racial justice that will help lessen health and economic disparities that have impaired communities of color for decades. “Climate action is a benefit multiplier,” he says. “It improves the health of every one of our patients, and it improves health equity in profound ways.”

DISEASE & DISRUPTED CARE
A planetary checkup
Climate change affects all aspects of human health, from presenting new opportunities for infectious diseases to flourish to exacerbating chronic diseases and stressing health care systems.

United States
Extreme weather events hinder access to care, especially for vulnerable populations. A team of researchers, including Harvard Chan’s Caroline Buckee and Rafael Irizarry, found that 30 percent of surveyed households in Puerto Rico reported interruptions to medical care in the wake of 2017’s Hurricane Maria, which left scores of families without water or electricity for weeks and killed thousands of people.
Sudan
Heat waves are becoming longer, more intense, and more frequent, and countries across North Africa and the Middle East are poised to endure some of the harshest extremes. Previous research from Harvard Chan’s Francesca Dominici indicates that heat waves caused by climate change may lead to increased deaths, especially in urban areas. Extreme heat can also make crops more prone to soilborne diseases and reduce agricultural yields.


Brazil
Rapacious clear-cutting of the Amazon rainforest is erasing precious carbon-storing green space. And, as research from Harvard Chan’s Marcia Castro has shown, it’s also driving malaria transmission by providing more favorable conditions for Anopheles mosquitoes.
Kiribati
Harvard Chan’s Chris Golden is analyzing how the decline of coral reefs and their fisheries—which are affected by an array of factors, including overfishing, wastewater leakage, ocean acidification, and warmer water temperatures—will impact the health of populations that depend on seafood as a key source of essential nutrients.

Australia
A historic string of wildfires in 2019 and 2020 scorched approximately 72,000 square miles, creating a smoke plume that scientists were able to track for more than 100 days. Research from several Harvard Chan scientists, including Samuel Myers, indicates that air pollution from wildfires is a serious threat to people with asthma, heart disease, and other health issues and is associated with increased mortality.
An emerging evidence base
For researchers studying the connections between climate risks and health risks, the more they look, the more they find.

Maternal heat exposure in early pregnancy can increase the risk of babies being born with congenital heart disease, according to research in the Journal of the American Heart Association. The study estimated that rising temperatures could result in 7,000 more children worldwide with congenital heart disease between 2025 and 2035.
Researchers reported in Nature Climate Change that increasing local temperatures and population densities are associated with increased antibiotic resistance in common pathogens, including Escherichia coli and Staphylococcus aureus. The researchers warned that current forecasts for antibiotic resistance could significantly underestimate the problem.
Patients whose radiotherapy treatments for advanced non–small cell lung cancer were interrupted by hurricanes—which scientists predict will become more frequent and more severe with increased climate change—had worse overall survival compared with patients who did not have a hurricane disaster declared during their treatment, according to a study in JAMA.
Seed idea
Build common ground
Talking about climate change can be difficult. Among other things, it requires navigating politics, countering misinformation, quelling anxieties, and overcoming apathy. But there is some good news. According to Harvard Chan C-CHANGE Interim Director Aaron Bernstein, research shows that focusing on health impacts is potentially one of the most effective ways to build common ground and support for climate action.
“By understanding climate change as a health issue, we can depoliticize it, make it actionable, and make it personal,” notes Bernstein, who is also a pediatrician at Boston Children’s Hospital. “And health care providers are some of the most trusted messengers in our society.”
Equipping doctors, nurses, and other clinicians to talk with patients about climate change when it’s relevant—explaining to allergy sufferers that research shows pollen seasons are getting longer, for instance—is only one part of the puzzle.
Bernstein says it’s equally important to get health care providers to recognize that climate change affects clinical practice—for instance, certain commonly prescribed medications may increase the odds of a person being hospitalized when the weather gets hot. “We need to be very clear that climate change is not merely a population health issue,” Bernstein says. “It’s an issue for health care delivery that affects access to care, the quality of care, and is very much relevant to how health care providers are able to do our jobs.”

PLATE & PLANET
Hungry for solutions
Our global food systems are bad for the environment and bad for human health. But planetary health expert Samuel Myers says there are plenty of fixes on the menu.
If you want a glimpse of how some of the planet’s biggest environmental, health, and social challenges intersect, take a stroll through the supermarket.
“There is an enormous planetary impact from our food production systems,” says Samuel Myers, principal research scientist for planetary health in the Department of Environmental Health and director of the Planetary Health Alliance. “We use 40 percent of the world’s ice-free terrestrial surface for crops and pasture. We use about half the accessible fresh water on the planet to irrigate crops. We fish 90 percent of our monitored fisheries at or well beyond maximum sustainable levels. We’ve cut down half the world’s forest, both tropical and temperate.”
It’s a system filled with feedback loops that jeopardize planetary health in myriad ways. Red meat, for example, is linked with increased risk of mortality from cardiovascular disease and cancer, and it’s a significant driver of pollution and climate change: Production of beef in the U.S. accounts for 36 percent of the country’s food-related emissions of greenhouse gases—gases that trap heat in the earth’s atmosphere and contribute to planetary warming. As carbon levels tick up, some of the world’s most essential staple crops—rice, wheat, barley—are becoming less nutritious. In a recent Nature Climate Change paper, Myers showed that concentrations of protein, iron, and zinc are 3 percent to 17 percent lower when crops are grown in environments where CO2 concentrations are 550 parts per million (ppm)—the projected level by 2050 if emissions continue at current rates—compared with crops grown under current atmospheric conditions of CO2 concentrations near 400 ppm.
“That puts hundreds of millions of people potentially at risk for deficiencies of essential nutrients,” Myers says. “And it’s a threat that disproportionately affects women and children in low-resource countries.”
But Myers says the impacts of our food system on planetary health extend far beyond carbon emissions. Myers has recently shifted his focus to the biodiversity crisis, how our food systems contribute to it, and the nutritional challenges it poses. “Thirty-six percent of the biomass of mammals on the planet is human beings. Sixty percent of the biomass is our livestock,” he says. “Only 4 percent is wild mammals.”

What does a diet look like that’s healthy for you and for the planet?
In 2019, the EAT-Lancet Commission on Food, Planet, Health, co-chaired by the Harvard Chan School’s Walter Willett, developed the world’s first scientific targets for a planetary health diet, along with this visual guide to help people understand what their daily diets should look like. The plant-forward diet emphasizes using unsaturated plant oils—olive oil, canola, peanut oil—over saturated oils such as palm or coconut oils. The diet also recommends limiting starchy vegetables such as potatoes and cassava to 50 grams a day, while prioritizing whole grains and plant-based proteins, such as nuts and seeds and legumes.
One of the big drivers of the so-called sixth extinction is changes in land use and land cover associated with food production. Carbon-absorbing forests have been cleared for carbon-producing dairy farms. Rivers have been dammed and drained. Overfarming has turned once-productive land into arid acreage. Neonicotinoid insecticides, which are also toxic to beneficial insects such as pollinators—have been dispensed on crops around the world. Such practices have swallowed up essential habitat and pushed scores of species to the brink. “There are a million species facing extinction, many within the next decade,” Myers says.
He’s especially concerned about how a rapid decline in pollinator insects will affect food production and has started collaborating on the issue with Lucas Garibaldi, an esteemed pollination ecologist at Argentina’s Universidad Nacional de Rio Negro. Garibaldi’s previous research found that a lack of pollinator species is responsible for a significant portion of the so-called yield gap—the difference in output between the highest-performing farms and average farms. Now Garibaldi, Myers, and colleagues are trying to connect the dots between the lost production of pollinator-dependent crops and the effects this loss will have on the global food trade and ultimately human health.
“Pollinator-dependent crops are mostly fruits, vegetables, nuts, seeds, and legumes, all of which play an important role in preventing noncommunicable diseases like heart disease, stroke, diabetes, and some forms of cancer,” Myers says. “We estimate that half a million deaths a year are attributable to inadequate pollination.”
The problem is only going to come into sharper focus as we continue to strive for diets that are healthier and better for the environment, because such diets require the exact type of foods that depend on pollinators. “There’s this big pollinator gap that no one’s talking about,” Myers says, “and we need to quantify it.”
Myers admits that confronting the overlapping health, climate, and environmental challenges of our food systems can seem overwhelming, but he says progress is being made every day. He recently edited a book on planetary health and wrote the chapter on food systems. Going into the project, he expected the focus to be on “whether we can get ourselves out of this mess.” But after analyzing the huge array of solutions available—from advances in precision agriculture to dietary changes to apps that reduce food waste by connecting consumers with grocery stores about to throw out food—he feels enormously optimistic. “The question isn’t ‘can we,’” he says. “The question is ‘will we?’”
Seed idea
Make school lunches greener
Before pursuing graduate studies in public health, Mary Kathryn Poole worked for a nonprofit organization, leading a project to improve the taste and palatability of meals at a Florida high school. The nutrition standards for the National School Lunch Program—which feeds more than 35 million schoolchildren a day and is a critical source of food for millions of low-income families—had undergone a historic update in 2010.
“Those standards led to major improvements in the nutritional quality of the meals and fostered innovation, like collaborations with chefs and from-scratch cooking,” she says. What they didn’t do was prioritize foods with low environmental impact.
That made Poole, now a PhD student in the Department of Nutrition, wonder: What would happen if U.S. school lunch standards aligned with benchmarks from the EAT-Lancet Commission on Food, Planet, Health (an initiative intended to reduce food systems’ contributions to climate change)? She analyzed data on 5,000 school lunches to consider how meals could be adjusted to improve nutrition and shrink the significant carbon footprint of the U.S. food system. The study, published in December 2020 in Health Affairs, revealed a dramatic underutilization of legumes and high levels of carbon-intensive meat and dairy. “We need to look for opportunities where nutrition and environmental health can align,” Poole says. “Redesigning school lunches could have a broad impact.”

Out of balance
Production of beef, dairy, and other animal-based food products is a major source of greenhouse-gas emissions. According to Samuel Myers, principal research scientist for planetary health, these agricultural practices also contribute significantly to the biodiversity crisis by swallowing up essential habitat and introducing harmful pesticides into the environment. The result is a world in which the amount of livestock far outweighs the amount of wild mammals left in nature.
Total mammalian biomass:
4%
wildlife
36%
wildlife
60%
wildlife
Source: Proceedings of the National Academy of Sciences
RENEWABLES RENAISSANCE
The future is electric
The days of the internal-combustion engine are numbered. Harvard Chan School researchers are studying how increased use of electric vehicles can improve public health and how drivers across all income levels can get charged up for the transition.
Will electric vehicles improve public health?
It’s finally safe to say that electric vehicles (EVs) are here to stay. Tesla has become a household name. General Motors announced in January that it will stop making cars that run on gasoline and diesel by 2035. The following month, Ford said it’s investing $22 billion in EVs and will offer only electric and plug-in models in Europe by 2026.

Electric vehicle charging station and instructions.
It’s an environmental win long in the making. But what exactly does it mean for public health? “The research is actually pretty scant,” says Ernani Choma, a postdoctoral research fellow in the Department of Environmental Health. “And one of the reasons is because it’s a very complicated question.”
Working with professors John Spengler, John Evans, and James Hammitt, Choma is developing methods to analyze how changes in vehicle emissions of specific air pollutants—such as fine particulates, sulfur dioxide, and nitrous oxide—affect the ambient concentration of fine particulate matter, which contributes to health conditions such as asthma and heart disease. Complicating the research is the fact that while EVs aren’t guzzling gas and belching greenhouse gases, the electricity on which they run is often generated by power plants that burn fossil fuels and pollute the air.
In a recently published Environment International paper, Choma and colleagues modeled how the switch to electric vehicles would affect mortality attributed to air pollution across 53 densely populated metropolitan areas in the U.S. In every city, uptake of electric vehicles was associated with significant drops in deaths attributed to air pollution, even when accounting for the increased electricity production at power plants.
Choma is quick to note that solutions such as public transportation systems, bike lanes, and walkable cities all need to be pursued. But given how ingrained driving culture is in America, EVs offer a significant opportunity to improve health and the environment. “Tackling climate change and reducing carbon emissions have been the driving force behind the push toward EVs,” Choma says. “Now we’re starting to show that the health benefits of EVs are also potentially huge in urban areas.”
Ok…but are they accessible?
The evidence in favor of EVs is mounting, and automakers are jumping into the market. But are consumers ready? Not exactly, according to a 2020 report from market research firm J.D. Power, which found consumer confidence in EVs is low and stagnant. Two of the most persistent barriers are charging station availability and “range anxiety,” or the fear that the battery will drain midtrip and leave a driver stranded.
“Anyone who has driven late at night and seen the low-gas light flick on knows that feeling, and it can be awful,” says Anne Lusk, a research scientist in the Department of Nutrition. Lusk, who holds a PhD in architecture, had previously studied how relatively modest design improvements in public parking lots could increase access to charging stations and help quell range anxiety. But given the direction of the EV market and the urgency of the climate crisis, she thinks we need to start thinking on a much grander scale about charging stations.
The solar energy equity gap
Installation of rooftop-solar energy varies sharply by race and ethnicity, according to an analysis of U.S. census tract data, which found:
69% lower
rate of rooftop-solar adoption in Black-majority census tracts compared with tracts that had no racial majority
30% lower
rate of rooftop-solar adoption in Hispanic-majority census tracts compared with tracts that had no racial majority
21% higher
rate of rooftop-solar adoption in white-majority census tracts compared with tracts that had no racial majority
Source: Nature Sustainability
“If we’re serious about ramping up adoption of EVs in the U.S.,” Lusk says, “then every home that has a parking space should have an electric vehicle charging post.”
It’s a bold idea that raises some big, important questions. For instance, Lusk points out that many homes that have an electric vehicle charging station tend to be higher-income and have the station located within a garage. “How many people who live in a city, where the health benefits of EVs are going to be greatest, have a garage?” Lusk asks. “How many low- and moderate-income people have access to their own garage?”
To help potential EV consumers explore the issue, Lusk recently launched a website that serves as a one-stop shop on all things EV, including how apartment buildings and condominiums could use networked chargers to improve charging access for renters and urban residents. “Having the ability to charge your car at your home or apartment is one of the best ways to overcome range anxiety,” Lusk says. “We need to start having these conversations now to help people think about how they want to adapt to EVs.”
Seed idea
Optimize renewables for health
“If you install a wind turbine, you are preventing asthma,” Jonathan Buonocore says. For a long time, however, the connection between renewable energy and public health benefits has been overlooked. Decisions on what type of renewable source to use and where to install it have been almost exclusively
about return on investment, not about where they’d have the greatest environmental or public health impact.
To make health an important part of the equation, Buonocore, a research scientist with Harvard Chan C-CHANGE, modeled 10 regions of the U.S. electrical grid and analyzed the health and climate benefits of air quality improvements associated with renewables. One of the most important findings: The type of renewable didn’t matter nearly as much as the location and the consequent energy sources it was offsetting.
In the Great Lakes region and Midwest, for instance, wind and solar were both associated with significant health benefits, but those gains were much lower in the Southwest. “One big reason why is because the Midwest has lots of high-emitting coal plants, some of which were built before the Clean Air Act went into effect and are upwind of major population centers. Renewables would displace those,” he says. “In the Southwest, it’s mostly newer natural gas systems that get displaced.”
With political and social winds shifting in favor of renewables, Buonocore’s model brings public health to the forefront of the conversation—and offers up a timely blueprint for cleaner air for everyone.